Overcoming Anxiety in pregnancy after previous miscarriages
Pregnancy should be a time of anticipation and joy, but for those who have experienced the heartbreak of miscarriages, it can also bring a shadow of anxiety and fear. If you’ve faced such losses, you’re not alone, and there are ways to navigate through this complex emotional landscape towards a place of hope and resilience.
Understanding Anxiety in Pregnancy
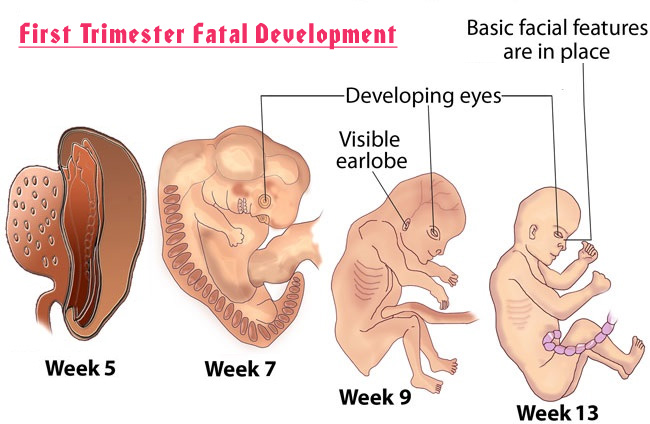
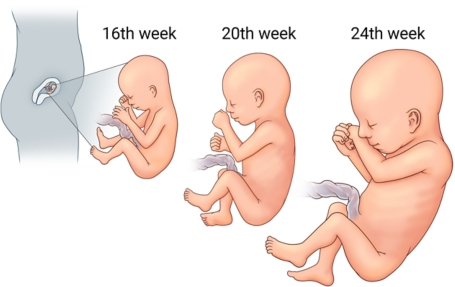
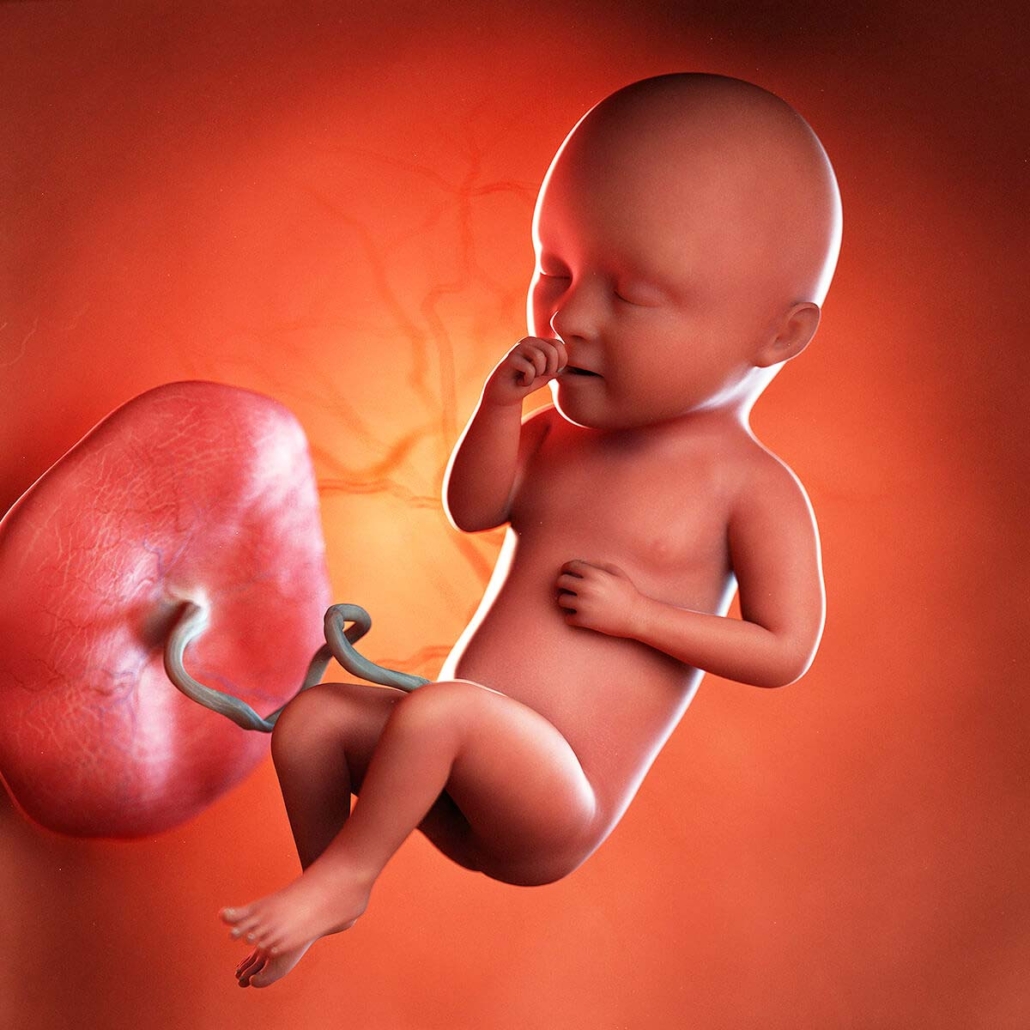
Anxiety during pregnancy, especially after previous miscarriages, is a natural response. It stems from the fear of the unknown and the desire to protect oneself from further emotional pain. However, it’s crucial to address this anxiety because it can affect both your well-being and that of your developing baby.
Strategies for Managing Anxiety
Seek Professional Support
One of the most effective steps you can take is to seek support from a healthcare provider who understands the nuances of pregnancy after loss. A therapist specializing in prenatal mental health can offer strategies tailored to your needs.
Build a Support Network
Surround yourself with people who understand what you’re going through. Support groups, both in-person and online, can connect you with others who share your experiences and fears.
Focus on What You Can Control
Focus on maintaining a healthy lifestyle, attending all prenatal appointments, and following your healthcare provider’s advice. Engaging in prenatal yoga or meditation can also help manage stress levels.
Educate Yourself
Understanding the facts about pregnancy after miscarriage can empower you. However, balance is key; too much information can sometimes increase anxiety.
Allow Yourself to Grieve and Heal
Recognize that it’s okay to grieve your losses even as you hope for the future. Acknowledging these emotions is a vital step toward healing.
Create a Plan with Your Healthcare Provider
Work with your healthcare provider to create a plan that addresses your concerns and outlines the steps to take should you encounter any issues during your pregnancy.
Practice Mindfulness and Relaxation Techniques
Mindfulness and relaxation techniques can be particularly beneficial in managing anxiety. Practices such as guided imagery, deep breathing exercises, and progressive muscle relaxation can help ground your thoughts in the present, reducing feelings of anxiety.
Supporting Data and External Links
- According to the American Pregnancy Association, mindfulness and relaxation techniques can significantly reduce stress and anxiety during pregnancy.
- The Miscarriage Association provides resources and support for those who have experienced loss, offering a community where your feelings are validated and understood.

Conclusion
Experiencing anxiety during pregnancy after miscarriages is a journey filled with mixed emotions. Yet, by employing strategies to manage anxiety, seeking support, and focusing on your well-being, you can navigate this path with greater peace and confidence. Remember, it’s okay to seek help, and it’s important to take care of yourself both physically and emotionally. Your feelings are valid, and there’s hope for a joyful outcome.
Let’s embrace this journey together, sharing stories of resilience and hope. If you’ve found particular strategies helpful, or if you have questions or concerns, please share them in the comments below. Your story can be a beacon of hope for others walking this path.
For further reading and resources, visit the American Pregnancy Association and The Miscarriage Association websites. These platforms offer valuable information and support networks to help you through this time.
Remember, you’re not alone on this journey. Together, we can navigate the complexities of pregnancy after loss, finding strength and hope in each other’s stories.
- American Pregnancy Association (Visit Here): Offers comprehensive information on pregnancy, including managing stress and anxiety during pregnancy, and provides resources for those who have experienced miscarriages.
- The Miscarriage Association (Visit Here): Provides support and information to anyone affected by miscarriage, ectopic pregnancy, or molar pregnancy. They offer resources that help individuals cope with grief and plan for future pregnancies.
Disclaimer
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. The purpose of this website is to promote broad consumer understanding and knowledge of various health topics. It is not intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition or treatment and before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.

 ToronTek
ToronTek