What Happens To A Woman’s Body During Childbirth
The human body is an amazing thing. It’s ability to fend off disease, perform essential functions, and harbor life until birth are a few of the most important, and amazing, feats that the human body is capable of. From the moment of conception, a woman’s body immediately begins to change in order to accommodate the internal growth of a child. As the pregnancy progresses, a woman’s body adapts to the needs of both the mother and child.
Childbirth is challenging and complications occur, but women’s bodies are designed to give birth. The shape of the pelvis, hormones, powerful muscles and more all work together to help you bring your baby into the world – before, during and after childbirth.
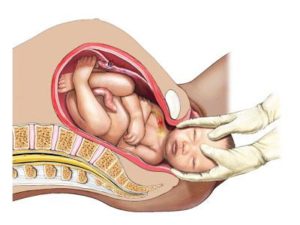
As you approach the time of birth, your contractions draw the cervix up into the body of the uterus, and it becomes thinner (called effacement) and opens (called dilation). When the cervix is fully dilated (about ten centimeters), contractions help the baby begin to move from the uterus into the vagina.
The First Trimester
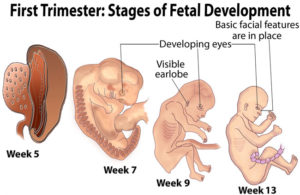 The first trimester is the time in between fertilization of the egg by the sperm (conception) and week 12 of a pregnancy. A woman’s body goes through many changes during the first 12 weeks of a pregnancy. a mother’s body is building storing nutrients and trying to keep up with the demands of a growing fetus. Fatigue is a normal reaction and is often the most inhibiting during the first trimester. Physical attributes may include constipation, heartburn, breast changes, and vaginal changes.
The first trimester is the time in between fertilization of the egg by the sperm (conception) and week 12 of a pregnancy. A woman’s body goes through many changes during the first 12 weeks of a pregnancy. a mother’s body is building storing nutrients and trying to keep up with the demands of a growing fetus. Fatigue is a normal reaction and is often the most inhibiting during the first trimester. Physical attributes may include constipation, heartburn, breast changes, and vaginal changes.
The Second Trimester 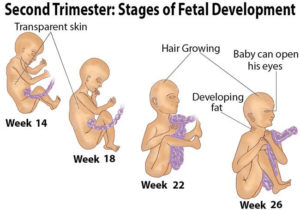
The second Trimester is the best part of pregnancy. The span from week 13 to week 27 of pregnancy is called the “honeymoon period” for good reason: Typically, nausea subsides, emotions even out and sex drive returns. It’s also the time when you’ll start to feel the baby’s first movements.
The Third Trimester
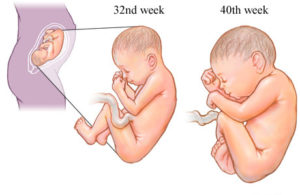 The third trimester of your pregnancy is from week 29 to week 40 – months seven, eight and nine.Your baby continues to grow, and as the third trimester progresses she’ll have a better chance if she’s born early. The end of your pregnancy is in sight. It won’t be long until your baby arrives. Feelings at this stage of pregnancy tend to vary from tiredness and worry to excitement about the baby.
The third trimester of your pregnancy is from week 29 to week 40 – months seven, eight and nine.Your baby continues to grow, and as the third trimester progresses she’ll have a better chance if she’s born early. The end of your pregnancy is in sight. It won’t be long until your baby arrives. Feelings at this stage of pregnancy tend to vary from tiredness and worry to excitement about the baby.
How does your body prepare for labor?
Braxton Hicks contractions
Braxton Hicks contractions are intermittent uterine contractions that start in early pregnancy, although you probably won’t notice them until sometime after mid-pregnancy. (Some women never notice them.) As your pregnancy progresses, Braxton Hicks contractions tend to occur somewhat more often, but until you get to your last few weeks, they’ll probably remain infrequent, irregular, and painless.
Changes to the cervix
As labor gets closer, your cervix softens and becomes thinner, getting ready for the dilation (widening) that will allow the baby to enter the vagina. You may also see a ‘show’ which is a pinkish plug of mucus, stained with blood.
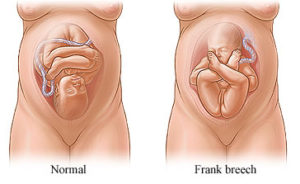
Engagement
Your baby may move further down your pelvis as the head engages, or sits in place over your cervix, ready for the birth. Some women feel they have more room to breathe after the baby has moved down. This is called ‘lightening’.
Rupture of the membranes, or ‘waters breaking’
Rupture of the membranes is known colloquially as “breaking the water” or as one’s “water breaking”. A premature rupture of membranes (PROM) is a rupture of the amnion that occurs prior to the onset of labor. Sometimes, a child is born with no rupture of the amniotic sac (no rupture of membranes).
Some women find the sac of amniotic fluid containing the baby breaks before labor, contractions start and the fluid runs (or gushes) out of the vagina. If your waters have broken but you have not started having regular contractions within 24 hours, you may need your labor to be induced because there is a risk of infection. Your midwife or doctor will talk to you about this.
How the pelvis is designed for childbirth 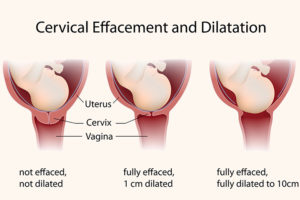
The female pelvis is the bony cradle that holds and even rocks your baby while she is developing in the uterus. It is amazingly designed for its functions, especially for giving birth.
The pelvis is well-designed to carry the weight of both the mother and baby. It connects the vertebrae and the lower limbs and protects the reproductive organs, the bladder, intestines, and rectum. It also provides attachment for the abdominal muscles and the muscles of the pelvic floor.
The pelvis is made up of four bones: the two large hip bones that form the sides of the cradle and meet at the front and the sacrum and coccyx at the back.
During pregnancy hormones cause the ligaments soften and stretch causing a slight separation of the joints, which allows flexibility for the baby’s head to pass through during birth. Sometimes pregnant women may experience some pelvic pain and discomfort as a result of this loosening of the joints.
The Childbirth Process
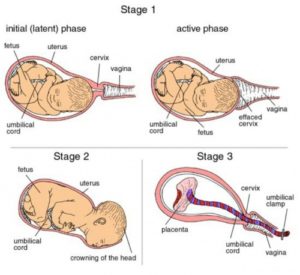 Childbirth, also known as labor and delivery, is the ending of a pregnancy by one or more babies leaving a woman’s uterus by vaginal passage or C-section. It involves three stages of labor: the shortening and opening of the cervix, descent, and birth of the baby, and the delivery of the placenta.
Childbirth, also known as labor and delivery, is the ending of a pregnancy by one or more babies leaving a woman’s uterus by vaginal passage or C-section. It involves three stages of labor: the shortening and opening of the cervix, descent, and birth of the baby, and the delivery of the placenta.
Cervical dilation occurs during active labor, making room for the baby to travel through the birth canal. The cervix dilates naturally when the body is ready to give birth, but when it’s necessary to move things along more quickly, dilation may be stimulated using medications or mechanical techniques.
The placenta is delivered as part of the afterbirth with a small gush of blood, from a few minutes to a half hour after the baby arrives. The doctor or midwife will examine it to make sure it’s intact and that nothing has been left behind in the uterus.
When childbirth doesn’t go to plan
Unfortunately, not everything goes to plan during birth. Sometimes your maternity team may need to intervene to assist in the delivery of your baby. Find out more about how your doctor or midwife may assist during your labor and what happens when your baby is premature or unwell.
Sometimes labor can be induced (started artificially) if your baby is overdue or there is any sort of risk to you or your baby’s health, for example, if you have high blood pressure or if your baby is failing to grow and develop.
In rare cases, a mother may experience cephalopelvic disproportion (CPD), which is when the baby’s head is too big to fit through the pelvis. A diagnosis of CPD is usually made when labor hasn’t progressed and synthetic oxytocin has not helped. A cesarean is usually the next step.
In conclusion, The stages of pregnancy and childbirth may seem daunting at times. However, they are some of the most rewarding phases of life. Bringing a child into this world is a beautiful labor.
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. The purpose of this website is to promote broad consumer understanding and knowledge of various health topics. It is not intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition or treatment and before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Resources:
https://www.pregnancybirthbaby.org.au/what-happens-to-your-body-in-childbirth
http://positivemed.com/2015/10/27/what-happens-to-a-womans-body-during-childbirth/