You’ve finally put 40 (or so) weeks of pregnancy and long hours of childbirth behind you, and you’re officially a mother. Congratulations! Now comes the transition from pregnancy to postpartum, which brings with it a variety of new symptoms and questions.
Your delivery may have been complicated or easy. You may have had a cesarean birth (C-section) or vaginal delivery. You may have labored for a few hours or a few days. No matter what your delivery looked like, your body has been through a trauma just the same. It is going to need time to recover.
How Long Does It Take to Recover After Giving Birth?
Your postpartum recovery won’t be just a few days. Fully recovering from pregnancy and childbirth can take months. While many women feel mostly recovered by 6-8 weeks, it may take longer than this to feel like yourself again. During this time, you may feel as though your body has turned against you. Try not to get frustrated. Remember that your body is not aware of your timelines and expectations. The best thing you can do for it is rest, eat well, and give yourself a break.
If you’ve had a vaginal birth, you’re probably also wondering how long it will take for the soreness to go away and your perineum to heal. Recovery can take anywhere from three weeks if you didn’t tear to six weeks or more if you had a perineal tear or an episiotomy. Wondering if your vagina will ever be the same after birth? Not exactly, though it will likely be very close.
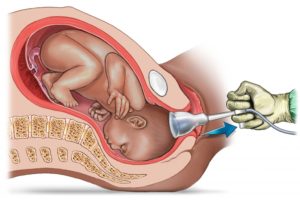
If you delivered by C-Section, expect to spend the first three to four days postpartum in the hospital recovering; it will take four to six weeks before you’re feeling back to normal. Depending on whether you pushed and for how long, you can also expect to have some perineal pain.
Here is more of what you can expect during your postpartum recovery
Abdominal pain. As your uterus shrinks back into its normal size and shape, you will feel pain in your abdomen (lower belly). These pains are called “afterpains.” Most of these pains will be dull, but some will be sharp. You may feel more of these pains as you breastfeed your baby. That is because breastfeeding stimulates a chemical in your body that causes the uterus to contract (tighten). For many women, applying heat to the area helps control the pain. Consider using a heating pad or hot water bottle. Your abdominal pain should ease up over time. If these pains get worse or don’t let up, you should call your doctor.
Baby blues. You are so excited and happy to bring baby home. The next minute, though, you are sad. It can be confusing, especially to new moms. Know that many women (70-80%) struggle with feeling sad the first few weeks after having a baby. It is commonly called the “baby blues” and is caused by hormone changes. It is nothing to be ashamed of. In fact, confiding in a friend of family member can often make you feel better. If these feelings last more than a few weeks or you are not able to function because of them, you could have postpartum depression. Postpartum depression is more serious than baby blues. If you have severe feelings of sadness or hopelessness, you should call your doctor.
Constipation. It is very common to be constipated in the days following childbirth. There are several things that could cause this. If you received any pain-relieving drugs in the hospital, they could slow down your bowels. If you had anesthesia (a pain blocker) for any reason, that also can cause it. Sometimes, postpartum constipation is brought on simply by fear. This is true especially if you have stitches because you had an episiotomy (a surgical cut between the vagina and anus to widen the vaginal opening for childbirth) or tore this area during delivery. You may be afraid of damaging the stitches or be afraid that a bowel movement will cause even more pain in that area. To help ease constipation, drink plenty of water and try to eat foods that offer a lot of fiber. In many cases, you may want to talk to your doctor about prescribing a stool softener (such as Colace or Docusoft). If you haven’t had a bowel movement by four days postpartum, call your doctor.
Hemorrhoids. You may have developed hemorrhoids (painful swelling of a vein in the rectum) during your pregnancy. If not, you may have gotten them from the strain and pushing during delivery. They can cause pain and bleed after a bowel movement. They also itch. You can get some relief from the pain and itching by applying witch hazel to your hemorrhoids. This is especially effective if you keep the witch hazel in the refrigerator. Your hemorrhoids should shrink over time. If not, contact your doctor.
Hormonal shifts. Besides fueling your mood swings (see “Baby blues,” above), hormones are also responsible for other postpartum symptoms. You may be sweating more, especially at night when you sleep. Just make sure that your sweating is not accompanied by a fever. That could be a sign of infection. Hormonal changes also cause hair loss for many new moms. This is only temporary. When your estrogen levels increase, your hair will return to its normal thickness.
Perineum soreness. The perineum is the area between your vagina and anus. Many times, this area will tear during childbirth. Other times, your doctor may have to make a small cut in this area to widen your vagina for childbirth. Even if neither of these things happened during your vaginal birth, you perineum will be sore and possibly swollen postpartum. You may feel discomfort in this area for several weeks. While you recover, sitting on an ice pack several times a day for 10 minutes will help relieve the pain. This is especially good to do after going to the bathroom. During the first week postpartum, also use a squirt bottle to rinse the perineum with warm water after using the toilet. Notify your doctor if your perineum area does not get less sore each day or you have any sign of infection.
Sore nipples and breasts. For achy breasts, try using a warm compress or ice packs and gentle massage. Also be sure to wear a comfortable nursing bra. If you’re breastfeeding, let your breasts air out after every nursing session and apply a lanolin cream to prevent or treat cracked nipples.
Stitches. If you have stitches due to a torn or cut perineum it will take 7-10 days to heal. The stitches will absorb over time. It is important that you keep the stitches from getting infected by gently cleaning them with warm water after each time you use the toilet. Do this by using a squirt bottle to rinse the area and pat it dry. Do not wipe the area with toilet paper or you could irritate the stitched area. No matter how eager you are to check the healing progress, try to keep your hands off the stitches. If the area begins to hurt worse or the stitches seem weepy, contact your doctor. It could be a sign of infection.
If you have stitches from a cesarean birth (C-section), these heal in varying degrees. The stitches in the skin should heal in 5-10 days. The underlying stitches in your muscle layer will take longer to heal. These won’t completely heal for 12 weeks. For the stitches that you can see, make sure to watch for any signs of infection. These signs include if the incision area is red, swollen, or weeping pus; or if you have a fever.
Vaginal bleeding and discharge. After you give birth, postpartum bleeding (this is called lochia) can last for up to six weeks. It will be just like a very heavy period made up of leftover blood, tissue from your uterus and mucus. Bleeding is heaviest for the first three to 10 days, then it will taper off going from red to pink to brown to yellowish-white. If you spot large clots or you’re bleeding through more than one pad every hour, call your doctor right away to rule out postpartum hemorrhage. During this time, tampons are off-limits, so you’ll have to rely on pads.
Water retention. You may be eager for that swelling you noticed during your pregnancy to go away. It won’t, though, for a while longer. Also known as postpartum edema (swelling), your body will continue to hold on to water because of an increase in a hormone called progesterone. You may notice the swelling in your hands, legs, and feet. It shouldn’t last much longer than a week after delivery. If it does or if it seems to get worse over time, be sure to tell your doctor.
Postpartum Recovery Checklist
Here are a few things you’ll want to make your postpartum recovery go as smoothly as possible:
- Acetaminophen. It can help with perineal pain and overall aches.
- Maxi pads. You’ll probably need these for at least a couple of weeks until postpartum bleeding lets up.
- Ice packs. There are lots of ways to ice your perineal area from frozen padsicles to your standard lunchbox ice blocks (wrapped in paper towels, of course, to avoid frostbite).
- Witch hazel pads. This is often used in combination with ice packs to ease vaginal pain and help with hemorrhoids.
- Sitz bath. This little tub is designed for you to just sit and soak away the postpartum pain.
- Peri or squirt bottle. You’ll use this to rinse off your perineal area before/after peeing as the area heals.
- Cotton underpants. Go for the “granny” or hospital gauze underwear, comfort is much more important for now than looking sexy.
- Nursing bras. Invest in a few comfy ones that fit you well.
- Lanolin. The cream works wonders to prevent and treat cracked nipples.
- Nursing pads. If you’re planning to breastfeed, these will help keep leaky nipples under wraps.
- Lidocaine spray. It helps ease the pain of postpartum hemorrhoids.
- Stool softener. In case you get stopped up, this can gently help get things going.
- Postpartum recovery belt. If you think you might want one, the Belly Bandit or other similar belts can help keep things in place as your belly shrinks back to size.
- Heating pad. This can help ease aches and pains in your breasts.
Things to consider
Pay attention to your body after giving birth. If something doesn’t seem right, it probably isn’t.
Just because you’ve made it through delivery, you are not necessarily out of danger for health complications. There are life-threatening problems related to childbirth that can happen days or weeks after delivery.
- Postpartum hemorrhage is rare but can happen. If your postpartum bleeding is filling more than a pad every hour, you should contact your doctor immediately. Without treatment, postpartum hemorrhage can be fatal.
- Headaches that are severe and don’t go away can also signal an underlying problem, especially coupled with high blood pressure. You could be in danger of having a stroke.
- Deep vein thrombosis (a blood clot in a deep vein) is a somewhat uncommon problem (1 in every 1,000 pregnancies) that can occur during or after pregnancy. Symptoms include leg pain or feeling like you have a pulled muscle. Your leg may also be red and hot to the touch. Left untreated, these clots can break away and travel to your lungs. When this happens, it can be life-threatening.
- Postpartum preeclampsia is rare and can develop within 48 hours after childbirth or as late as six weeks after childbirth. It is similar to preeclampsia (also called toxemia), which can occur while you’re pregnant. Both preeclampsia and postpartum preeclampsia cause your blood vessels to constrict (get smaller). This results in high blood pressure and also distresses your internal organs. Sometimes there are no obvious symptoms unless you are monitoring your blood pressure. When you do have symptoms, they may include a severe headache, swelling of your hands and feet, blurred vision, and sudden weight gain. If you suspect you may have postpartum preeclampsia, call your doctor immediately.
When to see a doctor
You’ll usually visit your doctor about 6 weeks after delivery. She’ll check your vagina, cervix, and uterus as well as your weight and blood pressure. Once you’ve gotten the all-clear from her, it’s usually fine to start having sex again (ask your doctor about birth control first) and to get back to an exercise routine.
Before your checkup, call your doctor right away if you have:
- Heavy vaginal bleeding that soaks more than one pad per hour or vaginal bleeding that increases each day instead of decreasing
- Passing large clots (bigger than a quarter)
- Chills and/or a fever of more than 100.4°F
- Fainting or dizziness
- Painful urination or difficulty urinating
- Vaginal discharge with a strong odor
- Heart palpitations, chest pain or difficulty breathing
- Vomiting
- The incision from C-section or episiotomy is red, weepy (with pus), or swollen
- Abdominal (lower belly) pain that is getting worse or new abdominal pain
- Sore breasts that are red or feel hot to the touch
- Pain in your legs with redness or swelling.
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. The purpose of this website is to promote broad consumer understanding and knowledge of various health topics. It is not intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition or treatment and before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Resources:
https://familydoctor.org/recovering-from-delivery/
https://www.webmd.com/parenting/baby/recovery-vaginal-delivery#3