What is Sleep apnea?
is a serious sleep disorder that occurs when a person’s breathing is interrupted during sleep. People with untreated sleep apnea stop breathing repeatedly during their sleep, sometimes hundreds of times. This means the brain — and the rest of the body — may not get enough oxygen. You may have sleep apnea if you snore loudly, and you feel tired even after a full night’s sleep.
“Sleep apnea can affect anyone at any age, even children.”
Types of sleep apnea:
- Obstructive sleep apnea, the more common form that occurs when throat muscles relax.
- Central sleep apnea, which occurs when your brain doesn’t send proper signals to the muscles that control breathing.
- Complex sleep apnea syndrome, also known as treatment-emergent central sleep apnea, occurs when someone has both obstructive sleep apnea and central sleep apnea.
If you think you might have any form of sleep apnea, see your doctor. Treatment can ease your symptoms and may help prevent heart problems and other complications.
Causes of Obstructive Sleep Apnea
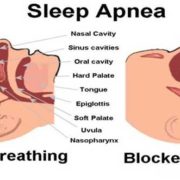
Obstructive sleep apnea occurs when the muscles in the back of your throat relax. These muscles support the soft palate, the triangular piece of tissue hanging from the soft palate (uvula), the tonsils, the side walls of the throat and the tongue.
When the muscles relax, your airway narrows or closes as you breathe in, and you can’t get an adequate breath in. This may lower the level of oxygen in your blood.
Your brain senses this inability to breathe and briefly rouses you from sleep so that you can reopen your airway. This awakening is usually so brief that you don’t remember it.
You may make a snorting, choking or gasping sound. This pattern can repeat itself five to 30 times or more each hour, all night long. These disruptions impair your ability to reach the desired deep, restful phases of sleep, and you’ll probably feel sleepy during your waking hours.
People with obstructive sleep apnea may not be aware that their sleep was interrupted. In fact, some people with this type of sleep apnea think they sleep well all night.
Symptoms
The signs and symptoms of obstructive and central sleep apneas overlap, sometimes making the type of sleep apnea more difficult to determine. The most common signs and symptoms of obstructive and central sleep apneas include:
- Loud snoring, which is usually more prominent in obstructive sleep apnea
- Episodes of breathing cessation during sleep witnessed by another person
- Abrupt awakenings accompanied by shortness of breath, which more likely indicates central sleep apnea
- Awakening with a dry mouth or a sore throat
- A morning headache
- Difficulty staying asleep (insomnia)
- Excessive daytime sleepiness (hypersomnia)
- Attention problems
- Irritability
- Forgetfulness, mood changes, a decreased interest in Sex
Risk factors for sleep apnea include:
- Being male. Men are twice as likely to have sleep apnea. However, women increase their risk if they’re overweight, and their risk also appears to rise after menopause.
- Being overweight. People who are obese have four times the risk of sleep apnea that people who are a normal weight people do. Fat deposits around your upper airway may obstruct your breathing. But not everyone who has sleep apnea is overweight.
- Being over age 40. Sleep apnea occurs significantly more often in older adults.
- Having a large neck size. (17 inches or greater in men and 16 inches or greater in women). People with thicker necks may have narrower airways.
- Having a family history. If you have family members with sleep apnea, you may be at increased risk.
- Smoking. Smokers are three times more likely to have obstructive sleep apnea than are people who’ve never smoked. Smoking may increase the amount of inflammation and fluid retention in the upper airway. This risk likely drops after you quit smoking.
Complications
Sleep apnea is considered a serious medical condition. Complications may include:
- Daytime fatigue. The repeated awakenings associated with sleep apnea make normal, restorative sleep impossible. People with sleep apnea often experience severe daytime drowsiness, fatigue, and irritability.
- You may have difficulty concentrating and find yourself falling asleep at work while watching TV or even when driving. People with sleep apnea have an increased risk of motor vehicle and workplace accidents.
- You may also feel quick-tempered, moody or depressed. Children and adolescents with sleep apnea may do poorly in school or have behavior problems.
- High blood pressure or heart problems. Sudden drops in blood oxygen levels that occur during sleep apnea increase blood pressure and strain the cardiovascular system. If you have obstructive sleep apnea, your risk of high blood pressure (hypertension) is greater than if you don’t.
- Obstructive sleep apnea may increase the risk of recurrent heart attack, and abnormal heartbeats, such as atrial fibrillation. Obstructive sleep apnea also increases the risk of stroke. If there’s underlying heart disease, these multiple episodes of low blood oxygen (hypoxia or hypoxemia) can lead to sudden death from an irregular heartbeat.
- Type 2 diabetes. People with sleep apnea are more likely to develop insulin resistance and type 2 diabetes compared with people without the sleep disorder.
- Metabolic syndrome. This disorder is a collection of other risk factors linked to a higher risk of heart disease. The conditions that make up metabolic syndrome include high blood pressure, abnormal cholesterol, high blood sugar and an increased waist circumference.
- Complications with medications and surgery. Obstructive sleep apnea is also a concern with certain medications and general anesthesia. People with sleep apnea may be more likely to experience complications following major surgery because they’re prone to breathing problems, especially when sedated and lying on their backs. Before you have surgery, tell your doctor that you have sleep apnea and how it’s treated.
- Liver problems. People with sleep apnea are more likely to have abnormal results on liver function tests, and their livers are more likely to show signs of scarring. This is a condition known as nonalcoholic fatty liver disease.
- Sleep-deprived partners. Loud snoring can keep those around you from getting good rest and eventually disrupt your relationships. It’s not uncommon for a partner to go to another room, or even on another floor of the house, to be able to sleep. Many bed partners of people who snore may be sleep-deprived as well.
Tests and Diagnosis
If you have symptoms of sleep apnea, your doctor may ask you to have a sleep apnea test, called a polysomnogram. This may be done in a sleep disorder center or even at home.
A polysomnogram or sleep study is a multiple-component test that electronically transmits and records specific physical activities while you sleep. The recordings are analyzed by a qualified sleep specialist to determine whether or another type of order sleep disorder.
If sleep apnea is determined, you may be asked to do further sleep testing in order to determine the best treatment option portable pulse oximeter can be very useful in monitoring your blood oxygen level (oxygen saturation) during sleep. In fact, the sleep apnea oximeter will show you how efficient is your apnea treatment.
What is a good oxygen level during sleep?
Oxygen saturation over 94% is considered normal. Anything below 92% oxygen in your blood is a sign that you have breathing problems during sleep (sleep apnea, severe snoring, COPD, asthma, etc).
However, is important to know how much time did you spend with oxygen saturation that goes below 92%.
There can be drops in oxygen levels that are not long enough or low enough to be called abnormal or unhealthy for your body. For example, a couple of seconds with 80% for 2 times in one night is not a reason for concern.
Pulse Oximeter for Sleep Apnea 
A pulse oximeter provides a record of your blood oxygen levels and heart rate while you wear the device. This information is very important to monitor the quality of your sleep, mostly if you know you have apnea episodes during sleep.
Sleep apnea pulse oximeters are expensive and generally not covered by insurance. However, finger pulse oximeters with recording capabilities can be found at much lower prices. http://torontek.com/product-category/oximeters/
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. The purpose of this website is to promote broad consumer understanding and knowledge of various health topics. It is not intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition or treatment and before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website
Resources:
https://www.webmd.com/sleep-disorders/sleep-apnea/diagnosing-sleep-apnea

 ToronTek
ToronTek