Insomnia During Pregnancy
/0 Comments/in Pegnancy tips, Pregnancy, Pregnancy Problem /by Rachel MataIt’s normal to have trouble sleeping at any point during pregnancy, but many expectant women experience insomnia starting in the second to third trimesters, as other pregnancy symptoms increase, and a burgeoning baby belly makes it harder than ever to get comfortable in bed.
Still, first trimester woes can force you from your cozy bed and disturb precious sleep too, including morning sickness, which can happen any time of the day or night, and a constant need to pee. But if you’re worried that a case of insomnia may harm your baby, rest assured it won’t. So do your best not to fret and sometimes, just letting go of these feelings is all it takes to help you sleep.
What is Insomnia?
Insomnia is a sleep disorder that makes it hard to drift off to sleep or stay asleep at night. This common sleep problem can also cause you to wake up too early and not be able to head back to dreamland, and it may make you feel as if the sleep you did manage to get wasn’t refreshing or restorative.
What Causes Insomnia During Pregnancy?
Insomnia during early pregnancy is usually due to factors such as hormonal changes. Many people experience insomnia at some point, during pregnancy. Better sleep hygiene, relaxation techniques, and cognitive behavioral therapy can help. Levels of the hormone progesterone are high during the first trimester, and this can cause sleepiness and napping during the day.
Aside from hormonal changes, factors that may make insomnia worse includes hunger, spicy foods, which may cause digestion issues, especially if eaten near bedtime, nausea, anxiety or depression, physical discomfort, and frequent bathroom trips. Other less obvious causes include difficulty breathing, with this difficulty sometimes affecting a person’s breathing at night when they are pregnant. This can cause snoring and brief pauses in breathing called apnea. Breathing problems during sleep at the end of the second and during the third trimester are more common.
Will Insomnia During Pregnancy Harm The Baby?
It’s understandable to assume that if you aren’t sleeping well, your baby isn’t either. But relax, your baby sleeps even when you’re wide awake. Your baby’s health is at risk, however, if your insomnia during pregnancy affects your ability to function. If you fall asleep while driving, or exhaustion leads you to stumble or fall, your baby could pay the price. Furthermore, research has found that women who have chronically disturbed sleep during pregnancy are at greater risk of gestational diabetes, preterm birth, depression, longer labor, and cesarean section. So it’s well worth doing what you can to sleep well.
What Can You Do To Improve Sleep During Pregnancy?
- Consider using a pregnancy pillow
- Diet and exercise
- Eat a healthy dinner
- Get a massage
- Establish good sleep habits.
- Create the ideal sleeping space
- Try to relax
Feeling exhausted is a common pregnancy symptom, particularly at the beginning and end of your pregnancy. However, if you always feel like you are finding yourself needing to sleep at all hours of the day, it may be time to speak with your doctor. They can make sure that no underlying medical conditions are causing this.
Disclaimer
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. The purpose of this website is to promote broad consumer understanding and knowledge of various health topics. It is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition or treatment before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
References:
https://www.healthline.com/health/pregnancy/excessive-sleeping-during-pregnancy#sleep-tips
https://www.healthline.com/health/pregnancy/early-insomnia#comfortis-key
Anxiety During Pregnancy
/0 Comments/in Health and wellness tip, Pegnancy tips, Personal, Pregnancy, Pregnancy Problem /by Rachel MataWhat is Anxiety?
Anxiety is feelings of worry, stress, or fear, and is a normal part of life. Anxiety is not only part of being pregnant, it’s part of being human. We all worry, and pregnancy can often amplify those worries. Antenatal anxiety is a very common experience. More than 1 in 10 women experience anxiety at some point during their pregnancy.
Pregnancy can be an incredibly wonderful time in your life, as well as a very scary time in your life. Pregnancy brings a mix of feelings, and not all of them are good. Your whole life as well as your body is going through a number of changes. These changes can be especially anxiety-provoking if this is your first pregnancy. You want everything to go perfectly, but you find yourself struggling with an array of worries and fears about every possible thing that could go wrong. If you’re feeling worried, you’re not alone. Worry is common, especially during a woman’s first pregnancy or an unplanned one. It can be even harder if you’re dealing with depression or anxiety. The more you think about those things, the worse your anxiety becomes.
What causes anxiety during pregnancy?
Pregnancy is also a time of tremendous change and hormonal changes during pregnancy may affect the chemicals in your brain. This can cause anxiety. After all, not everything that makes you feel anxious is under your control. Some of these feelings and sensations are welcomed, while others are downright uncomfortable and scary. You may even have complications or other issues that arise that keep you up at night.
What Are Some Symptoms of Anxiety During Pregnancy?
Since there are different types of anxiety disorders, the symptoms vary. Speak with your doctor about any symptoms you experience so he or she can accurately diagnose and treat you. Some common symptoms of anxiety disorders include:
- feeling an uncontrollable sense of anxiousness
- worrying excessively about things, especially your health or baby
- feeling irritable or agitated
- having tense muscles
- Feeling nervous, anxious or on edge frequently
- Finding it difficult or impossible to relax
- Feeling restless and hard to stay still
- Feeling afraid, or thinking that bad things will happen
- Inability to concentrate
- Difficulty sleeping
Things You Can Do to Manage Your Anxiety
- Avoid Scary Stories and Images
- Stop Thinking of “What Ifs”
- Meditate
- Deep-breathing exercises
- Avoid Stress
- Find a release
- Talk about it
- Rest up
Treatment for Anxiety During Pregnancy
- Counseling or therapy
- Support groups
- Medication
- Other approaches
- Exercise
- Eating a healthy diet
- Get enough sleep
- Meditate and breathe
When to See a Doctor?
Even if you experience only mild symptoms of anxiety, it is important to inform your doctor. If your anxiety is affecting your daily life or if you’re having frequent panic attacks, you should call your doctor right away. Only they can diagnose you with an anxiety disorder and recommend the best, most effective treatment options for you. Seeking help is the best step you can take to ensure that you and your child stay safe and healthy. The sooner you get help, the sooner you’ll be able to gain peace of mind for your health and the health of your growing baby.
Always remember; Take care of yourself as much as you can, for your and your baby’s health. Be sure to eat well, exercise, get enough sleep, and take your prenatal vitamins. Look for ways to reduce your stress.
Disclaimer
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. The purpose of this website is to promote broad consumer understanding and knowledge of various health topics. It is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition or treatment and before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
References:
https://www.healthline.com/health/pregnancy/anxiety-coping-tips#treatment
Foods to Eat and Avoid During Pregnancy
/0 Comments/in Health and wellness tip, Pegnancy tips, Pregnancy /by Rachel MataFoods to Eat and Avoid During Pregnancy
It’s well known that a mother’s diet during pregnancy is very important to the health of her baby. Expecting mothers need to consume more vitamins, minerals, and other nutrients that are helpful for a fetus’s growth and development. However, there are also some foods pregnant women should avoid. There are some foods you should not eat when you’re pregnant because they might make you ill or harm your baby. Certain foods should only be consumed rarely, while others should be avoided completely. Make sure you know the important facts about which foods you should avoid or take extra care with when you’re pregnant. The best foods to eat are freshly cooked or freshly prepared food.

5 foods to eat during pregnancy
- Produce containing Vitamin C, like oranges, strawberries, bell peppers, and broccoli, support the baby’s growth and improves iron absorption. Adding in servings of green veggies is an efficient way to pack in vitamins and fend off constipation due to all that fiber. Vegetables rich diets linked means reduced risk of low birth weight.
- Foods that have iron, such as beans, lentils, green leafy vegetables, Lean beef, pork, chicken, and spinach are excellent sources of high-quality protein and all support the mother’s body in making more blood for both mom and baby. Red blood cells use iron as a part of hemoglobin, an essential mineral.
- Dairy products. During pregnancy, you need to consume extra protein and calcium to meet the needs of your growing little one. Dairy products like milk, cheese, and yogurt should be on the docket. Foods rich in calcium, including pasteurized dairy products (yogurt, cow’s milk, and hard cheeses) as well as almonds, broccoli, and garbanzo beans will help support the development of bones and teeth. Dairy products contain two types of high-quality protein: casein and whey. Dairy is the best dietary source of calcium and provides high amounts of phosphorus, B vitamins, magnesium, and zinc.
- Foods containing Omega-3 fatty acids (EHA and DHA) such as sardines, salmon, trout, and canned light tuna. Or choose a prenatal supplement with Omega-3s if you don’t like fish.
- Drinking plenty of water to stay hydrated supports the proper delivery of nutrients through the blood to the baby. Increasing your water intake may also help relieve constipation and reduce your risk of urinary tract infections, which are common during pregnancy. We all have to stay hydrated and pregnant especially. During pregnancy, blood volume increases by about 45 percent. General guidelines recommend that pregnant women drink about 80 ounces (2.3 liters) of water daily. But the amount you really need varies. Check with your doctor for a recommendation based on your specific needs.

5 foods to avoid during pregnancy
- Anything containing unpasteurized milk, however, is a no-no. These products could lead to foodborne illness. Avoid soft cheeses, such as brie, feta, and blue cheese, unless they are clearly labeled as being pasteurized or made with pasteurized milk. Also, avoid drinking unpasteurized juice.
- Any food in a dented can increases the risk for botulism, a foodborne illness that can cause neuromuscular deficits for expecting mothers.
- Avoid raw, undercooked, or contaminated seafood. Consuming raw seafood, like sushi or raw oysters, increases the risk of salmonella, a foodborne illness that can cause fever and nausea, vomiting, stomach cramping, and diarrhea for pregnant women, as well as intrauterine sepsis that can affect babies.
- Avoid seafood high in mercury. Fish with a high mercury content, such as swordfish, shark, orange roughy, marlin, and king mackerel. Too much mercury could harm your baby’s developing nervous system
- Avoid Alcohol during pregnancy. There is nothing as safe level of alchol during pregnancy. The safest bet is to avoid alcohol entirely. Drinking alcohol during pregnancy leads to a higher risk of miscarriage and stillbirth. Drinking alcohol may also result in fetal alcohol syndrome, which can cause facial deformities and intellectual disability.
Disclaimer
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. The purpose of this website is to promote broad consumer understanding and knowledge of various health topics. It is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition or treatment before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
References:
Headaches During Pregnancy
/0 Comments/in Health and wellness tip, Pegnancy tips, Pregnancy, Pregnancy Problem /by Rachel MataHeadaches during pregnancy
If you’re pregnant, you’re no doubt experiencing new aches and pains. Headaches can be common in early pregnancy. They usually improve as your pregnancy goes on. Headaches in women can often be triggered by a change in hormones during pregnancy. Expectant mothers may experience an increase or decrease in the number of headaches. A headache can sometimes be a symptom of pre-eclampsia, which can lead to serious complications if it’s not monitored and treated. Pre-eclampsia usually starts after 20 weeks of pregnancy. Nearly all women have occasional headaches, but having a headache in pregnancy is not fun, especially tricky in the first trimester when you should avoid many medicines. Whether your headache is from tension or is a full-blown migraine, there are some things you should know.
What causes headaches during pregnancy?
The exact cause of a headache isn’t always clear. In the first trimester, changing hormone levels and blood volume may play a role. Hunger and low levels of blood sugar can trigger headaches, too. Researchers believe that overly excited brain cells stimulate a release of chemicals. These chemicals irritate blood vessels on the brain’s surface. That, in turn, causes blood vessels to swell and stimulate the pain response. Headaches during your second or third trimester of pregnancy may be a sign that you have high blood pressure. About 6 to 8 percent of pregnant women ages 20 to 44 in the United States have high blood pressure.
Other causes of headaches during pregnancy can include:
- not getting enough sleep
- hormonal changes
- withdrawal from caffeine (e.g. in coffee, tea, or cola drinks)
- low blood sugar
- dehydration
- feeling stressed
- poor posture, particularly as your baby gets bigger
- having depression or anxiety
- weight changes
- high blood pressure
Types of headaches
Most headaches during pregnancy are primary headaches. This means that the headache pain happens by itself. It’s not a sign or symptom of another disorder or a complication in the pregnancy. Primary headaches include:
- Tension headaches: A tension-type headache (TTH) is generally a mild to moderate pain that’s often described as feeling like a tight band around the head. About 26 percent of headaches during pregnancy are tension headaches and are common in the first trimester of your pregnancy.
- Migraine attacks: Migraine headaches are a common type of headache in pregnancy. These painful, throbbing headaches are usually felt on one side of the head and result from the expansion of the blood vessels in the brain.
- Cluster headaches: Cluster headaches are one of the most painful types of headaches. A cluster headache commonly awakens you in the middle of the night with intense pain in or around one eye on one side of your head.
What can I do about headaches?
Steps to manage headaches include the following:
- Avoid any known headache triggers
- Include physical activity in your daily routine.
- Reduce your stress level and relax
- Practice relaxation techniques.
- Eat regularly
- Follow a regular sleep schedule.
- drink plenty of fluids to prevent dehydration
- get enough sleep
Treatment for headaches during pregnancy
If you experience frequent headaches that don’t go away with paracetamol, it could be a sign of a more serious medical condition called pre-eclampsia. Most pregnant women can safely take acetaminophen (Tylenol, others) to treat occasional headaches. Talk to your doctor before taking your regular headache pain medication during pregnancy.
See your doctor if you have any headache pain at all during pregnancy. Get urgent medical attention if you have a fever, severe pain, and blurred vision. Let your doctor know right away.
Disclaimer
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. The purpose of this website is to promote broad consumer understanding and knowledge of various health topics. It is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition or treatment before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
References:
https://www.healthline.com/health/pregnancy/headache-during-pregnancy#treatment
https://www.webmd.com/migraines-headaches/migraines-headaches-finding-help
Using Epidural Anesthesia During Labor: Benefits and Risks
/0 Comments/in Child birth, Delivery, Pegnancy tips, Pregnancy /by Rachel MataUsing Epidural Anesthesia During Labor: Benefits and Risks
Epidural anesthesia is a regional anesthesia that blocks pain in a specific part of the body, making it the most preferred method of pain relief during labor. Women request it by name more than any other pain relief method. The primary aim of an epidural is to provide analgesia, or pain relief, rather than total anesthesia, which results in a complete absence of sensation. Epidurals work by blocking nerve impulses from the lower spinal segments, and over 50% of women in hospitals opt for this type of anesthesia during childbirth.
Types of epidurals?
Regular Epidural: Once the catheter is positioned, a mix of a narcotic and an anesthetic is delivered either through a pump or by periodic injections into the epidural space. To supplement the higher doses of anesthetic required, narcotics such as fentanyl or morphine are used.
Combined Spinal-Epidural (CSE) or “Walking Epidural”: An initial dose of narcotic, anesthetic, or both is injected into the intrathecal space, located just beneath the outermost membrane covering the spinal cord and deeper than the epidural space. After this, the anesthesiologist retracts the needle to the epidural space, inserts a catheter through the needle, removes the needle, and leaves the catheter in place for continuous pain relief. This method offers more mobility in bed and the ability to change positions with assistance. You can request additional epidural pain relief through the catheter if needed. Generally, CSE provides pain relief for 4-8 hours.
Benefits of Epidurals During Delivery
- Potential for a painless delivery.
- Allows rest during prolonged labor.
- Can enhance the childbirth experience by reducing discomfort.
- Essential for cesarean delivery, enabling you to remain awake and providing effective pain relief during recovery.
Risks of Epidurals During Delivery
- Low blood pressure: Approximately 14% of women experience a drop in blood pressure with an epidural, which is typically not harmful. Healthcare professionals will monitor your blood pressure closely, administering fluids and medication as needed to maintain it.
- Loss of bladder control: The epidural may numb the nerves around your bladder, making it difficult to sense when it’s full. A catheter may be inserted to manage urination until the epidural’s effects wear off.
- Nausea and vomiting: Opioid pain relievers used in epidurals can cause nausea and vomiting as side effects.
- Fever: About 23% of women with an epidural develop a fever, compared to 7% without one. The cause of the temperature increase is unclear.
- Permanent nerve damage: Although rare, there’s a slight risk of permanent sensory or motor loss in the legs.
Other complications
Very rare complications include seizures, severe breathing difficulties, and in extremely rare cases, death.
When is an epidural NOT an option?
- If taking certain medications
- With heavy bleeding or low platelet counts
- In the presence of an infection on or near the back
- If experiencing hemorrhage or shock
- Labor is progressing too rapidly
- The epidural space cannot be located
- Inadequate dilation (less than 4 cm)
- Abnormal blood work
Considerations and Restrictions:
Discuss the benefits and risks of epidural anesthesia with your anesthetist to make an informed decision. While epidurals offer significant pain relief, they come with potential side effects. Your decision should be based on your personal pain tolerance and preferences.
Disclaimer
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. The purpose of this website is to promote broad consumer understanding and knowledge of various health topics. It is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition or treatment before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
References:
https://www.healthline.com/health/pregnancy/natural-birth-vs-epidural
https://www.healthline.com/health/pregnancy/pain-risks-epidurals
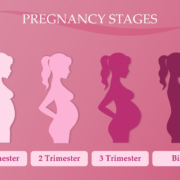
Stages of Pregnancy
/0 Comments/in Child birth, Health and wellness tip, Pegnancy tips, Pregnancy /by Rachel MataStages of Pregnancy
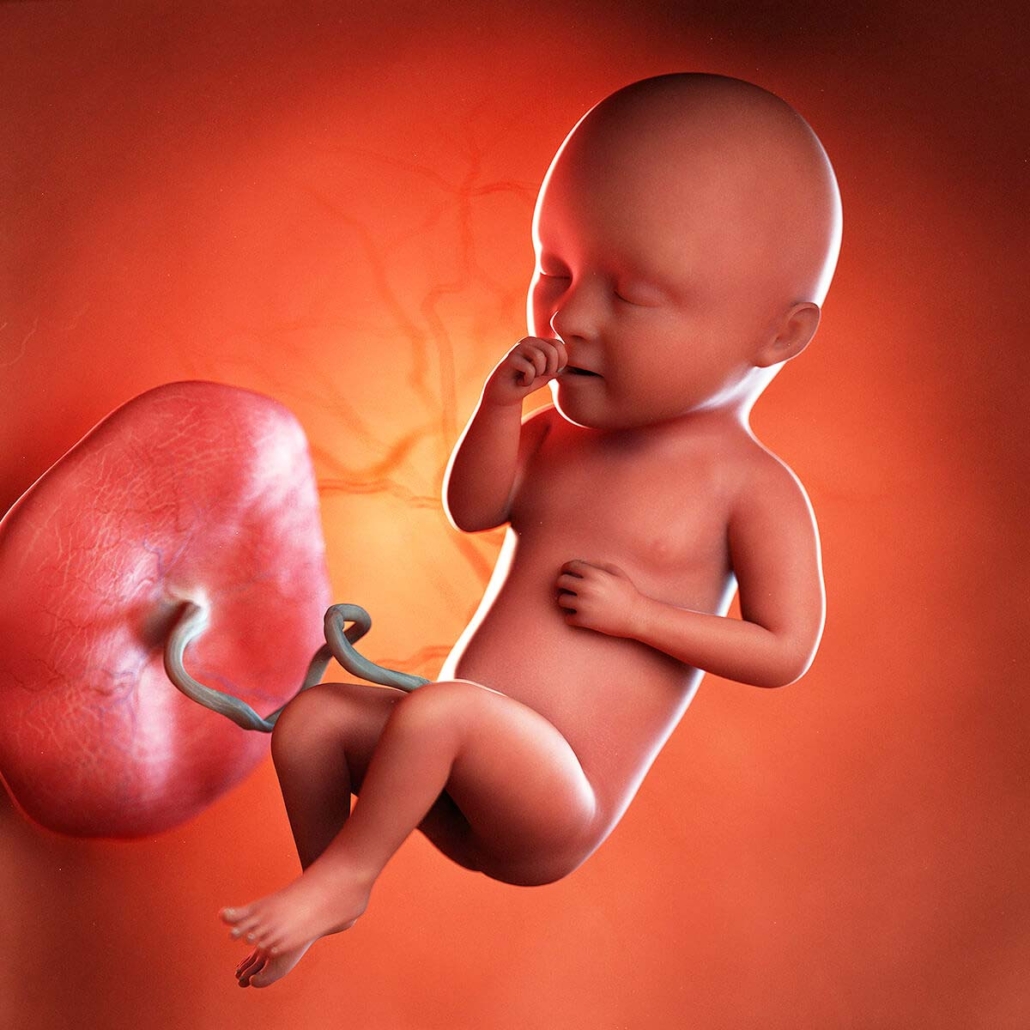
Within 24 hours after fertilization, the egg that will become your baby rapidly divides into many cells. By the eighth week of pregnancy, the embryo develops into a fetus. Pregnancy is counted as 40 weeks, starting from the first day of the mother’s last menstrual period. These weeks are divided into three trimesters. Your estimated date of birth is only to give you a guide. Babies come when they are ready and you need to be patient. Below we explore the stafes of pregnancy:
Pregnancy is divided into three trimesters:
- First trimester – conception to 12 weeks
- Second trimester – 12 to 24 weeks
- Third trimester – 24 to 40 weeks.
The moment of conception is when the woman’s ovum (egg) is fertilized by the man’s sperm to complete the genetic make-up of a human fetus. At this moment (conception), the sex and genetic make-up of the fetus begin. About three days later, the fertilized egg cell divides rapidly and then passes through the Fallopian tube into the uterus, where it attaches to the uterine wall. The attachment site provides nourishment to the rapidly developing fetus and becomes the placenta.
The start of Stages of Pregnancy?
Medical professionals measure pregnancy week 1 from the first day of a woman’s last menstrual period. This is called the gestational age, or menstrual age. It’s about two weeks ahead of when conception actually occurs. Although a woman is not actually pregnant at this point, counting week 1 from the last menstrual period can help determine a woman’s estimated pregnancy due date. Your healthcare provider will ask you about this date and will use it to figure out how far along you are in your pregnancy.
How early can I know I’m pregnant?
From the moment of conception, the hormone human chorionic gonadotrophin (hCG) will be present in your blood. This hormone is created by the cells that form the placenta (food source for the growing fetus). It’s also the hormone detected in a pregnancy test. While you may get a positive POAS test at 3 weeks, it’s a good idea to wait a week or two and test again to confirm. A blood test also can detect hCG and is more sensitive than a urine test. Pregnancy can detect pregnancy as early as 6 days after ovulation, you could be able to confirm your pregnancy at/around 3 weeks.
Stages of Fetal Development
During the first trimester, your body undergoes many changes. Hormonal changes affect almost every organ system in your body. These changes can trigger symptoms even in the very first weeks of pregnancy. Your period stopping is a clear sign that you are pregnant.
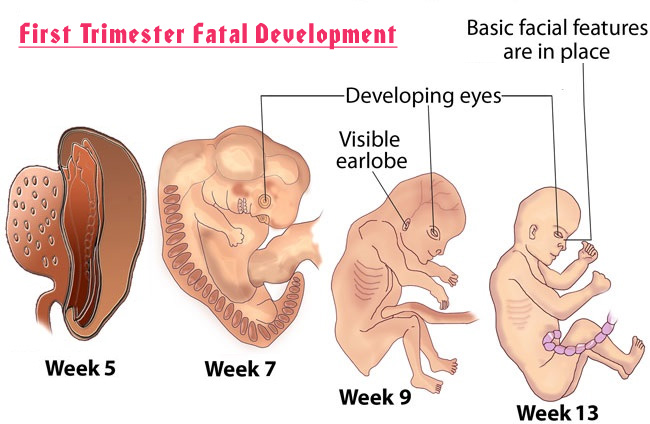
The developing baby is tinier than a grain of rice. The rapidly dividing cells are in the process of forming the various body systems, including the digestive system. The evolving neural tube will eventually become the central nervous system (brain and spinal cord).
First trimester (week 1–week 12)
- 1 and 2: Getting ready
- 3: Fertilization
- 4: Implantation
- 5: Hormone levels increase
- 6: The neural tube closes
- 7: Baby’s head develops
- 8: Baby’s nose forms
- 9: Baby’s toes appear
- 10: Baby’s elbows bend
- 11: Baby’s genitals develop
- 12: Baby’s fingernails form
Second trimester (week 13–week 27)
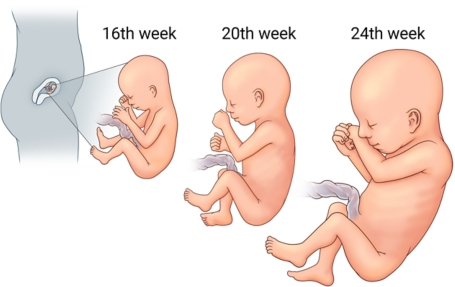
Most women find this second trimester easier than the first. But it is just as important to stay informed during all stages of pregnancy.
You might notice that symptoms like nausea and fatigue are going away. But other new, more noticeable changes to your body are now happening. Your abdomen will expand as the baby continues to grow. And before this trimester is over, you will feel your baby beginning to move. Fetal development takes on new meaning in the second trimester. Highlights might include finding out your baby’s sex and feeling your baby move.
- 13: Urine forms
- 14: Baby’s sex becomes apparent
- 15: Baby’s scalp pattern develops
- 16: Baby’s eyes move
- 17: Baby’s toenails develop
- 18: Baby begins to hear
- 19: Baby develops a protective coating
- 20: The halfway point
- 21: Baby can suck his or her thumb
- 22: Baby’s hair becomes visible
- 23: Fingerprints and footprints form
- 24: Baby’s skin is wrinkled
- 25: Baby responds to your voice
- 26: Baby’s lungs develop
- 27: At 27 weeks, or 25 weeks after conception, your baby’s nervous system is continuing to mature. Your baby is also gaining fat, which will help his or her skin look smoother.
Third trimester (week 28–week 40)
Some of the same discomforts you had in your second trimester will continue. Plus, many women find breathing difficult and notice they have to go to the bathroom even more often. This is because the baby is getting bigger and it is putting more pressure on your organs. Your baby will open his or her eyes, gain more weight, and prepare for delivery.
- 28: Baby’s eyes partially open
- 29: Baby kicks and stretches
- 30: Baby’s hair grows
- 31: Baby’s rapid weight gain begins
- 32: Baby practices breathing
- 33: Baby detects light
- 34: Baby’s fingernails grow
- 35: Baby’s skin is smooth
- 36: Baby takes up most of the amniotic sac
- 37: Baby might turn head down
- 38: Baby’s toenails grow
- 39: Baby’s chest is prominent
- 40: Your due date arrives
As you near your due date, your cervix becomes thinner and softer (called effacing). This is a normal, natural process that helps the birth canal (vagina) to open during the birthing process. Your doctor will check your progress with a vaginal exam as you near your due date. Get excited as the final countdown has begun.
Don’t be alarmed if your due date comes and goes with no signs of labor starting. Your due date is simply a calculated estimate of when your pregnancy will be 40 weeks. It does not estimate when your baby will arrive. It’s normal to give birth before or after your due date.
Disclaimer
The information on stages of pregnancy, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. The purpose of this website is to promote broad consumer understanding and knowledge of various health topics. It is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition or treatment before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Preferences:
https://my.clevelandclinic.org/health/articles/7247-fetal-development-stages-of-growth
Pregnancy Fatigue
/0 Comments/in Health and wellness tip, Pegnancy tips, Personal, Pregnancy /by Rachel MataPregnancy Fatigue
Fatigue during pregnancy is very common. Some women may feel exhausted throughout their pregnancy, while some may hardly feel tired at all. One of the first signs of pregnancy is fatigue. Fatigue can begin in the very first weeks of pregnancy. It’s common to feel tired, or even exhausted, during pregnancy. Hormonal changes taking place in your body at this time can make you feel nauseous and emotional – affecting your body, mood, and sleep. Although experience with fatigue tends to vary, most women will feel more tired than usual during their pregnancy, and it is most common during the first trimester. It tends to go away during the second trimester, but will usually return in the third trimester.
What causes Pregnancy Fatigue?
It’s common to feel tired, or even exhausted, during pregnancy, especially in the first 12 weeks. Hormonal changes at this time can make you feel tired, nauseous, and emotional. The only answer is to rest as much as possible.
Causes of pregnancy fatigue for the first trimester:
- Building the placenta
- Your hormones
- Increased blood supply.
- Other physical changes
By the end of the first trimester, your body will have completed the enormous task that saps your body of energy on manufacturing the placenta and grown a bit more used to the hormonal and emotional changes that have occurred, which means the second trimester is usually a time of renewed energy levels.
During your second trimester, there is a good chance your energy level will increase and you will start to feel more like your old self. The second trimester is often called “The Happy Trimester.” Fatigue during pregnancy is still possible during the second trimester.
Causes of pregnancy fatigue for the third trimester:
- Your growing baby bump
- Pregnancy insomnia and other symptoms
- The stress of having a baby
- Multi-tasking
During the third trimester, you will most likely begin to feel tired again. At this point you will be carrying extra weight from the baby, maybe having trouble sleeping, and dealing with pregnancy demands.
Coping tips for Pregnancy Fatigue
- Make sure you allow yourself to get enough bed rest during the times you feel fatigued
- Eat healthy meals and stay hydrated. Try to look after your physical health by eating a healthy diet, and doing some gentle exercise. Eating nutritious meals will go a long way toward supporting your energy levels. Make sure you get enough iron, protein, and calories. Fatigue can become worse if you are not getting the proper nutrients. Make sure you stay hydrated during your pregnancy.
- Take time to exercise, if you incorporate moderate activity, such as a 30-minute walk, this will actually make you feel more energized. Exercise is beneficial in pregnancy unless your healthcare provider has advised otherwise.
Pregnancy can be a tiring experience, both emotionally and physically. It’s important to remember. You are not alone. Know that all of these pregnancy conditions are manageable and treatable, but you need to keep the communication lines open with your doctor.
Have a Happy, Healthy Pregnancy
Disclaimer
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. The purpose of this website is to promote broad consumer understanding and knowledge of various health topics. It is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition or treatment before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Exercising During Pregnancy
/0 Comments/in Health and wellness tip, Pegnancy tips, Pregnancy, Pregnancy Problem /by Rachel MataExercising During Pregnancy
All women who are pregnant without complications should be encouraged to keep up their normal daily physical activity or strength-conditioning exercises as part of a healthy lifestyle during their pregnancy. Pregnancy might seem like the perfect time to sit back and relax. You likely feel more tired than usual, and your back might ache from carrying extra weight. Exercise is not dangerous for your baby. There is some evidence that active women are less likely to experience problems in later pregnancy and labor. The more active and fit you are during pregnancy, the easier it will be for you to adapt to your changing shape and weight gain. Maintaining a regular exercise routine throughout your pregnancy can help you stay healthy and feel your best. It will also help you to cope with labor and get back into shape after the birth.
Who Should Not Exercise During Pregnancy?
For those that have medical problems, such as asthma, heart disease, diabetes, low placenta, bleeding or spotting, previous premature births, or a history of early labor, exercise may not be advisable.
Talk with your doctor before beginning an exercise program. They can also give you personal exercise guidelines, based on your medical history.
What Exercises Are Safe During Pregnancy?
Most exercises are safe to perform during pregnancy, as long as you exercise with caution and do not overdo it. Do not exhaust yourself. You may need to slow down as your pregnancy progresses.
- Dancing
- Swimming
- Water aerobics
- Yoga, stretching, and other floor exercises
- Pilates
- Biking
- Brisk walking
- Indoor stationary cycling
- pregnancy exercise classes
As a general rule, you should be able to hold a conversation as you exercise when pregnant. If you become breathless as you talk, then you’re probably exercising too strenuously.
Exercise tips during pregnancy
If you have been cleared to exercise, and you participated in physical activity before you were pregnant, it is recommended that you:
- Always warm up before exercising, and cool down afterward
- At least 30 minutes of moderate-intensity physical activity, try to keep active on a daily basis
- Listen to your body. Let your body be your guide.
- If you are healthy and you are not experiencing complications in your pregnancy, continue this level, or until it becomes uncomfortable for you to do so.
- Drink plenty of water and other fluids
- Try swimming because the water will support your increased weight.
- Consult and be guided by your doctor, physiotherapist, or healthcare professional.
Benefits of exercise during pregnancy
- Reduce backaches, constipation, bloating, and swelling
- Boost your mood and energy levels
- Help you sleep better
- Prevent excess weight gain
- Promote muscle tone, strength, and endurance
- Decreased risk of pregnancy complications such as pre-eclampsia and pregnancy-induced hypertension
- Faster recuperation after labor
- Prevention and management of urinary incontinence
- Improved circulation
- Lower risk of gestational diabetes
- Shortened labor
- Reduced risk of having a C-section
Exercises to avoid while pregnant
- abdominal trauma or pressure; such as weightlifting
- Activities where falling is likely (such as skiing and horseback riding).
- extreme balance, coordination, and agility; such as gymnastics
- significant changes in pressure – such as SCUBA diving
- heavy lifting
- wide squats or lunges.
- Holding your breath during any activity.
- Activities that require extensive jumping, hopping, skipping, bouncing, or running.
- Deep Knee bends, full sit-ups, double leg raises, and straight-leg toe touches.
- Waist-twisting movements while standing.
- Heavy exercise spurts followed by long periods of no activity.
- Exercise in hot, humid weather.
Warning signs when exercising during pregnancy
Stop exercising and consult your health care provider if you:
- Feel chest pain
- Have a headache
- dizziness or feeling faint
- heart palpitations
- chest pain
- swelling of the face, hands, or feet
- calf pain or swelling
- vaginal bleeding
- contractions
- deep back, pubic or pelvic pain
- cramping in the lower abdomen
- an unusual change in your baby’s movements
- amniotic fluid leakage
- unusual shortness of breath
- excessive fatigue
- muscle weakness
Regular exercise can help you cope with the physical changes of pregnancy and build stamina for the challenges ahead. If you haven’t been exercising regularly, use pregnancy as your motivation to begin. If you’re not sure whether a particular activity is safe during pregnancy, check with your healthcare professional. Always talk to your doctor before beginning any exercise program. Once you’re ready to get going.
Disclaimer
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. The purpose of this website is to promote broad consumer understanding and knowledge of various health topics. It is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition or treatment before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
References:
https://kidshealth.org/en/parents/exercising-pregnancy.html
Chia Seeds During Pregnancy
/0 Comments/in Health and wellness tip, Pegnancy tips, Pregnancy /by Rachel MataWhat are Chia Seeds?
Chia is as super for pregnant women as it is for everyone else. Chia seeds are tiny edible seeds that contain several vital nutrients. They are full of fiber and packed with Omega 3 fatty acids and antioxidants. These little seeds contain calcium, phosphorus, magnesium, and protein and these are important for bone health. Since these nutrients promote overall health, consuming chia seeds during pregnancy can benefit you and your baby. This is a great seed for healthy living.
Is it safe to eat chia seeds during pregnancy?
Some people wonder whether chia seeds are safe to eat while pregnant or breastfeeding. Chia seeds are safe to consume during pregnancy and can actually boost the chances of a healthy delivery. Many expecting mothers wonder how much chia seeds should be consumed daily. Knowing this is essential as excessive intake of these seeds can have certain side effects that may affect you and the baby. Around 100g of chia seeds provide approximately 20g of protein. Consuming 1 tablespoon of chia seeds can provide you with 3g of protein. Chia seeds also contain iron and calcium, both of these minerals are essential for a healthy pregnancy. These vitamins are great for both you and your baby while pregnant.
Benefits of chia seeds in pregnancy
- Relief from constipation: Chia seeds are loaded with insoluble fiber that aids digestion. It can, therefore, treat constipation, a common complaint during pregnancy.
- Can boost your red blood cells
- Can strengthen baby’s teeth and bones: Chia seed is a good source of Calcium which will ensure proper skeletal development of your baby and even help build his tooth buds.
- Can help prevent anemia.Blood sugar regulation: The fiber in chia seeds can slow down the absorption of sugar in your blood and keep it stable, thereby lowering the risk of Type 2 diabetes and heart disease
- Can help you stay full longer: So whenever possible, add a few sprinkles of chia seeds to your recipes.The more protein-rich foods you eat, the less hungry you’ll feel.
- A good source of omega-3: Omega-3 helps reduce chronic inflammation, contributes to eye health, and even eases anxiety and depression. It also promotes healthy brain development in unborn babies and may even contribute to a healthy pregnancy
- Can help promote fetal development: Chia seeds are a healthy source of protein, which is an extremely important nutrient during pregnancy as it promotes the development of organs (including the brain) and cells of the fetus.
- May give more energy: As a healthy fat, chia seeds may give you a much-needed pick-me-up. The seeds aren’t going to eliminate fatigue; they’re a superfood, not a miracle cure.
- Improves oxygen supply: Chia contains Iron that is essential for the production of extra red blood cells that carry oxygen to the body system. Chia seeds are one of the easiest ways to get this nutrient into your diet.
Risks of Chia Seeds in pregnancy
- stomach discomfort can result from eating too much – Chia seeds are healthy and natural, but this doesn’t mean you can’t overdo it.
- Chia seeds are blood thinners and may lower your blood pressure and cause bleeding.
- Possible drug interactions do exist – although chia seeds regulate blood sugar levels, they may interact with certain drugs and medication.
- May trigger allergic reactions – Chia seeds may also trigger allergic reactions like rashes, hives, and watery eyes.
How to Consume Chia Seeds
- Chia seeds with water
- Chia seeds smoothie
- Chia Seeds Sandwich
- Chia seed pudding
- Chia protein pancakes
Chia seeds are a necessity for pregnant women due to their high protein content and excellent nutrition profile. Chia seeds might be small in size, but there’s nothing insignificant about their nutritional punch. They are nutritious, and they are safe to consume while pregnant or breastfeeding. So whether you’re looking for a bit more energy or you want to try getting rid of constipation, go ahead and sprinkle some chia seeds over your food. And don’t stop eating the seeds just because you’ve given birth; their health benefits are for everyone. We recommend that you speak to your doctor and find out whether they interfere with your existing medications before you begin incorporating them into your diet. As always, add one to two tablespoons of chia seeds a day during pregnancy and you’ll be all set for your pregnancy.
Disclaimer
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. The purpose of this website is to promote broad consumer understanding and knowledge of various health topics. It is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition or treatment before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
References:
https://www.momjunction.com/articles/chia-seeds-during-pregnancy_00446553/
https://www.healthline.com/health/pregnancy/chia-seeds-pregnancy https://www.medicalnewstoday.com/articles/chia-seeds-pregnancy#benefits
https://www.medicalnewstoday.com/articles/chia-seeds-pregnancy#benefits