Multiple Pregnancy
A multiple pregnancy is when you are pregnant with twins, triplets or more. Three babies or more is called a ‘higher order’ pregnancy, and it’s rare – occurring in just 1 in 50 multiple pregnancies.
Having twins, triplets or more can be challenging, but most families find having several babies at once a positive experience.
How does multiple pregnancy occur? 
Multiple pregnancies occur when more than one embryo implants in your uterus (womb). This can happen if you release more than one egg during the menstrual cycle and each egg is fertilized by a sperm. Sometimes, a fertilized egg spontaneously splits into 2, resulting in identical embryos. This type of pregnancy results in fraternal twins (or more). When a single fertilized egg splits, it results in multiple identical embryos. This type of pregnancy results in identical twins (or more). Identical twins are less common than fraternal twins.
What are some causes of multiple pregnancy?
The use of fertility drugs to induce ovulation often causes more than one egg to be released from the ovaries and can result in twins, triplets, or more. Multiple pregnancies are more common than they used to be, mainly because of the increasing use of in vitro fertilization (IVF) if more than one embryo is transferred to the uterus. Identical multiples also may result if the fertilized egg splits after transfer. Women aged 35 and older are more likely to release more than one egg during ovulation, so they are more likely to have a multiple pregnancy. You are also more likely to have a multiple pregnancy if you have a history of twins in your family.
What are some symptoms of multiple pregnancy?
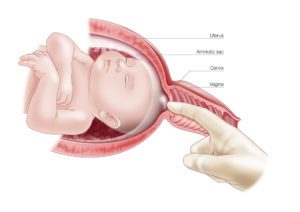
Women who are pregnant with multiples may have more severe morning sickness or breast tenderness than women who are pregnant with a single baby. They also may gain weight more quickly. A multiple pregnancy is confirmed by an ultrasound scan, usually in the first trimester (the first 12 weeks). The ultrasound will confirm the type of multiple pregnancy, whether there is one placenta or 2, and how many amniotic sacs there are. These are all important factors for later in the pregnancy and it’s important to identify them as early as possible.
Types of multiple pregnancy
Fraternal twins 
Two separate eggs are fertilized and implant in the uterus. The babies are siblings who share the same uterus – they may look similar or different, and may either be the same gender (2 girls or 2 boys) or of different genders. A pregnancy with fraternal twins is statistically the lowest risk of all multiple pregnancies since each baby has its own placenta and amniotic sac. You will sometimes hear fraternal twins referred to as ‘dizygotic’ twins, referring to 2 zygotes (fertilized eggs).
Identical twins
 Identical twins are formed when a single fertilized egg is split in half. Each half (embryo) is genetically identical, so the babies share the same DNA. That means the babies will share many characteristics. However, because their appearance is influenced by the environment as well as by genes, sometimes identical twins can look quite different. Identical twins may share the same placenta and amniotic sac, or they may have their own placenta and amniotic sac. You will sometimes hear identical twins referred to as ‘monozygotic’, referring to one zygote (fertilized egg).
Identical twins are formed when a single fertilized egg is split in half. Each half (embryo) is genetically identical, so the babies share the same DNA. That means the babies will share many characteristics. However, because their appearance is influenced by the environment as well as by genes, sometimes identical twins can look quite different. Identical twins may share the same placenta and amniotic sac, or they may have their own placenta and amniotic sac. You will sometimes hear identical twins referred to as ‘monozygotic’, referring to one zygote (fertilized egg).
Triplets and ‘higher order multiples’ (HOMs)
Triplets, quadruplets, quintuplets, sextuplets or more can be a combination both of identical and fraternal multiples. For example, triplets can be either fraternal (trizygotic), forming from 3 individual eggs that are fertilized and implanted in the uterus; or they can be identical, when one egg divides into 3 embryos; or they can be a combination of both.
Do I need to gain extra weight if I am pregnant with multiples?
It generally is recommended that women who are pregnant with multiples gain more weight than women who are pregnant with one baby. An extra 300 calories a day is needed for each fetus. For instance, if you are pregnant with twins, you need an extra 600 calories a day. For triplets and higher-order pregnancies, weight gain should be individualized.
Complications of Multiple Pregnancy
The most common complications include the following: 
- Preterm labor and birth. Over 60% of twins and nearly all higher-order multiples are premature (born before 37 weeks). The higher the number of fetuses in the pregnancy, the greater the risk for early birth. Premature babies are born before their bodies and organ systems have completely matured. These babies are often small, with low birth weights (less than 2,500 grams or 5.5 pounds), and they may need help breathing, eating, fighting infection, and staying warm. Very premature babies, those born before 28 weeks, are especially vulnerable. Many of their organs may not be ready for life outside the mother’s uterus and may be too immature to function well. Many multiple birth babies will need care in a neonatal intensive care unit (NICU).
- Gestational hypertension. Women with multiple fetuses are more than twice as likely to develop high blood pressure of pregnancy. This condition often develops earlier and is more severe than pregnancy with one baby. It can also increase the chance of placental abruption (early detachment of the placenta).
- Anemia. Anemia is more than twice as common in multiple pregnancies as in a single birth.
- Birth defects. Multiple birth babies have about twice the risk of congenital (present at birth) abnormalities including neural tube defects (like spina bifida), gastrointestinal, and heart abnormalities.
- Miscarriage. A phenomenon called the vanishing twin syndrome in which more than 1 fetus is diagnosed, but vanishes (or is miscarried), usually in the first trimester, is more likely in multiple pregnancies. This may or may not be accompanied by bleeding. The risk of pregnancy loss is increased in later trimesters as well.
- Twin-to-twin transfusion syndrome. Twin-to-twin transfusion syndrome (TTTS) is a condition of the placenta that develops only with identical twins that share a placenta. Blood vessels connect within the placenta and divert blood from one fetus to the other. It happens in about 15% of twins with a shared placenta.
In TTTS, blood is shunted from 1 fetus to the other through blood vessel connections in a shared placenta. Over time, the recipient fetus receives too much blood. This can overload the cardiovascular system and cause too much amniotic fluid to develop. The smaller donor fetus does not get enough blood and has low amounts of amniotic fluid. TTTS can be treated during pregnancy by withdrawing some of the extra fluid with a needle or with surgery on the placenta. Sometimes, the twins may need to be delivered early.
- Cerebral Palsy: A long-term disability of the nervous system that affects young children in which control of movement or posture is abnormal and is not the result of a recognized disease.
- Abnormal amounts of amniotic fluid. Amniotic fluid abnormalities are more common in multiple pregnancies, especially for twins that share a placenta.
- Cord entanglement. Cord entanglement for the twins that share the amniotic sac. In these cases, monitoring of the fetuses often in the third trimester may be necessary.
- Cesarean delivery. Abnormal fetal positions increase the chances of cesarean birth.
- Postpartum hemorrhage. The large placental area and over-distended uterus place a mother at risk for bleeding after delivery in many multiple pregnancies.
Can multiple pregnancy affect my risk of postpartum depression? 
Multiple births increase the risk of postpartum depression. Multiple births are a risk factor for postpartum depressive symptoms in mothers. If you have intense feelings of sadness, anxiety, or despair that prevent you from being able to do your daily tasks, let your obstetrician or other members of your health care team know.
Can I breastfeed if I have multiples?
Yes, but it may take some practice. Your milk supply will increase the right amount. You will need to eat healthy foods and drink plenty of liquids. The law of supply and demand applies to nursing mothers of twins and multiples. If you breastfeed when your babies want to eat, you can trust your body to supply enough milk. A low milk supply can almost always be corrected by nursing more often. If your babies aren’t emptying your breasts, you may need to pump.
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. The purpose of this website is to promote broad consumer understanding and knowledge of various health topics. It is not intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition or treatment and before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Resources: