A typical pregnancy lasts about 40 weeks, yet some babies arrive sooner. Babies born before the 37th week of gestation are considered premature. Premature newborns are sometimes referred to as “preemies”. Mothers who have their baby prematurely are often frightened and nervous. Premature newborns face an increased risk of one or more complications.
While some premature babies have serious medical complications or long-term health problems, many also go on to live normal healthy lives. With modern medicine and new technologies, babies are often able to survive when born earlier during the pregnancy.
The Most Common Complications of Premature Births
Breathing problems 
Breathing problems in premature babies are caused by an immature respiratory system. Immature lungs in premature babies often lack surfactant. This substance is a liquid that coats the inside of the lungs and helps keep them open. Without surfactant, a premature baby’s lungs can’t expand and contract normally. This increases their risk for respiratory distress syndrome.
Some premature babies who lack surfactant may need to be put on a ventilator (breathing machine). Babies who are on a ventilator for a long time are at risk of developing a chronic lung condition called bronchopulmonary dysplasia. This condition causes fluid to build up in the lungs and increases the likelihood of lung damage.
Transient tachypnea is rapid shallow breathing. This can occur in both premature babies as well as full-term babies. Recovery usually takes three days or less. Until the newborn has recovered, feedings may be altered, and in some cases, intravenous feedings may be done. There is usually no other treatment necessary.
apnea and Bradycardia – Apnea is the absence of breathing. In the NICU an alarm will sound if a newborn develops an irregular breathing pattern of pauses longer than 10-15 seconds. Bradycardia is the reduction of heart rate.
An alarm will also sound if the newborn’s heart rate falls below 100 beats per minute. Usually, a little tap or simple rub on the back helps remind the preemie to breathe and also increases the heart rate.
Treatment: While being on a ventilator for an extended period of time may injure a baby’s lungs, it still may be necessary for the baby to receive continued oxygen therapy and ventilator support. Doctors may also use diuretic and inhaled medications.
Jaundice 
The most common type of jaundice among premature babies is exaggerated physiologic jaundice. In this condition, the liver can’t rid the body of bilirubin. This substance is produced during the normal breakdown of red blood cells. As a result, bilirubin accumulates in the baby’s blood and spreads into the tissues. Because bilirubin is a yellowish color, the baby’s skin takes on a yellowish tint.
Jaundice is usually not a serious problem. However, if the bilirubin level gets too high, it can cause bilirubin toxicity. The substance can then build up in the brain and cause brain damage.
Ask your doctor or nurse for your baby’s bilirubin level. Normal levels of bilirubin in a newborn should be under 5 mg/dL. Many preterm babies, however, have bilirubin levels above that number. Bilirubin levels are not dangerous until they reach levels above 15-20 mg/dL, but phototherapy is generally started before levels get that high.
Treatment: The standard treatment for jaundice is phototherapy. This involves placing a baby under bright lights. The lights help break down the bilirubin into a substance that the body can get rid of more easily. Usually phototherapy is needed for less than a week. After that, the liver is mature enough to get rid of bilirubin on its own.
Kidney problems
A baby’s kidneys usually mature quickly after birth, but problems balancing the body’s fluids, salts, and wastes can occur during the first four to five days of life. This is especially true in babies less than 28 weeks into development.
During this time, a baby’s kidneys may have difficulty:
- filtering wastes from the blood
- getting rid of wastes without excreting excess fluids
- producing urine
Because of the potential for kidney problems, neonatal intensive care unit (NICU) staff carefully record the amount of urine a baby produces. They may also test the blood for levels of potassium, urea, and creatinine.
Staff must also be watchful when giving medications, especially antibiotics. They need to make sure that the medicines are excreted from the body. If problems arise with kidney function, staff may need to restrict the baby’s fluid intake or give more fluids so that substances in the blood are not overly concentrated.
Treatment: The most common basic treatments are the fluid restriction and salt restriction. Immature kidneys usually improve and have a normal function within a few days.
Infections
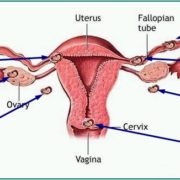
A premature baby can develop infections in almost any part of the body. A baby may acquire an infection at any stage, ranging from in utero (while in the uterus), birthing through the genital tract, to after birth including the days or weeks in the NICU.
Regardless of when an infection is acquired, infections in premature infants are more difficult to treat for two reasons:
- A premature baby has a less developed immune system and fewer antibodies from the mother than a full-term baby. The immune system and antibodies are the body’s main defenses against infection.
- A premature baby often requires a number of medical procedures, including insertion of intravenous (IV) lines, catheters, and endotracheal tubes and possibly assistance from a ventilator. Each time a procedure is performed, there’s a chance of introducing bacteria, viruses, or fungi into the baby’s system.
If your baby has an infection, you may notice some or all of the following signs:
- lack of alertness or activity
- difficulty tolerating feedings
- poor muscle tone
- inability to maintain body temperature
- pale or spotted skin color, or a yellowish tint to the skin (jaundice)
- slow heart rate
- apnea (periods when the baby stops breathing)
These signs may be mild or dramatic, depending on the severity of the infection. As soon as there’s any suspicion that your baby has an infection, the NICU staff obtains samples of blood and often urine and spinal fluid to send to the laboratory for analysis.
Treatment: If there is evidence of infection, your baby may be treated with antibiotics, IV fluids, oxygen, or mechanical ventilation (help from a breathing machine). Although some infections can be serious, most babies respond well to treatments, including antibiotics if the infection is bacterial. The earlier your baby is treated, the better the chances of successfully fighting the infection.
Heart problems
The most common heart condition affecting premature babies is called a patent ductus arteriosus (PDA). The ductus arteriosus is the opening between two major blood vessels of the heart. In premature babies, the ductus arteriosus may remain open (patent) instead of closing as it should soon after birth. If this occurs, it can cause extra blood to be pumped through the lungs in the first days of life. Fluid can build up in the lungs, and heart failure can develop.
Treatment: Babies can be treated with the medication indomethacin, which causes the ductus arteriosus to close. If the ductus arteriosus remains open and symptomatic, an operation to close the duct may be required.
Brain problems 
Brain problems can also occur in premature babies. Some premature babies have intraventricular hemorrhage, which is bleeding in the brain. Mild bleeding doesn’t usually cause permanent brain injury. However, heavy bleeding may result in permanent brain injury and cause fluid to accumulate in the brain. Severe bleeding can affect a baby’s cognitive and motor function.
Treatment: Treatment for brain problems can range from medication and therapy to surgery, depending on the severity of the problem.
Long-term complications
Some premature birth complications are short-term and resolve within time. Others are long-term or permanent. Long-term complications include the following: 
- Cerebral palsy: Cerebral Palsy is a movement disorder that affects muscle tone, muscle coordination, movement, and balance. It’s caused by an infection, poor blood flow, or a brain injury during pregnancy or after birth. Often, a specific cause can’t be determined.
- Vision problems: Premature babies are at risk for retinopathy of prematurity. In this condition, blood vessels in the back of the eye become swollen. This can cause gradual retina scarring and retinal detachment, increasing the risks of vision loss or blindness.
- Hearing problems: Some premature babies experience some hearing loss. Hearing loss can sometimes be total, causing deafness. Many times, the exact cause hearing loss in premature babies is unknown.
- Dental problems: Dental issues can affect a premature baby later in life. These include tooth discoloration, delayed tooth growth, or improper alignment.
- Behavioral problems: Children born prematurely are more likely to have behavioral or psychological problems. These include attention-deficit disorder (ADD) and attention-deficit/hyperactivity disorder (ADHD).
- Impaired cognitive function: Premature babies are also at greater risk for long-term disabilities, which can be intellectual, developmental, or both. These children may develop at a slower rate than babies born full-term.
- Chronic health problems: In addition, premature babies have a greater risk for chronic health problems. They are more susceptible to infections and may suffer from other problems such as asthma or difficulty feeding. There’s also an increased risk of sudden infant death syndrome (SIDS) among premature infants.
Survival Rate
The earlier a baby is born, the greater the risk for short-term and long-term complications.
Length of pregnancy and Survival rate:
- 34+ weeks = Almost the same rates as a full-term baby
- 32-33 weeks = 95%
- 28-31 weeks = 90-95%
- 27 weeks = 90%
- 26 weeks = 80%
- 25 weeks = 50%
- 24 weeks = 39%
- 23 weeks = 17%
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. The purpose of this website is to promote broad consumer understanding and knowledge of various health topics. It is not intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition or treatment and before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Resources:
https://www.healthline.com/health/pregnancy/premature-baby-complications#longterm-complications
http://americanpregnancy.org/labor-and-birth/premature-birth-complications/