Preeclampsia: Prevention, Management, and Risks
Preeclampsia is a pregnancy disorder that involves high blood pressure rises higher than 140/90 mm Hg after week 20 of your pregnancy along with other symptoms,You also may be tested for protein in your urine because of stress on your kidneys. Other names for preeclampsia include toxemia, pregnancy-induced hypertension (PIH), and gestosis. Preeclampsia is one of four hypertensive disorders of pregnancy and this condition could seriously hurt you and your baby, if you don’t receive treatment, it can harm your brain, kidneys, and liver. You can also develop eclampsia, which can put both your lives at risk.
It may ease your mind to know you can greatly reduce the risk of preeclampsia by going to all your prenatal appointments. In fact, most pregnant women who have preeclampsia have healthy babies.
Learn why you are at risk and what you can do to have the safest pregnancy possible.
Am I at Increased Risk?
Up to 8% of pregnancies are affected by preeclampsia.
Your risk for developing preeclampsia is greater if you have a history of:
- High blood pressure before pregnancy
- Preeclampsia or high blood pressure during a past pregnancy
- Diabetes or kidney disease
- An autoimmune disorder such as rheumatoid arthritis, scleroderma, or lupus
You are also at increased risk if you:
- Are a teen or older than age 40
- Obesity
- First pregnancy
- Twin/multiple pregnancy
- Donor egg pregnancies
- Family history of preeclampsia
How Does Preeclampsia Affect Pregnant Women?
If preeclampsia is not treated quickly and properly, it can lead to serious complications for the mother such as liver or renal failure and future cardiovascular issues.
Because preeclampsia affects many organ systems in the body, increased blood pressure is only one of many symptoms that may be present. Other symptoms of preeclampsia include increased protein in the urine and generalized swelling.
In some women, preeclampsia becomes very severe. Signs that the condition is worsening should be reported to your doctor immediately and include:
- Reduced urine output
- Trouble with vision
- Abdominal pain
- Headache
- Nausea/vomiting
- Seizures
It may also lead to the following life-threatening conditions:
- Eclampsia– This is a severe form of preeclampsia that leads to seizures in the mother.
- HELLP Syndrome (hemolysis, elevated liver enzymes, and low platelet count)- This is a condition usually occurring late in pregnancy that affects the breakdown of red blood cells, how the blood clots, and liver function for the pregnant woman.
How Does Preeclampsia Affect Babies?
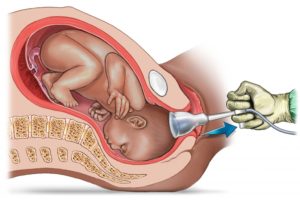
Preeclampsia affects babies primarily by reducing the amount of blood that flows through the placenta. Because the placenta is the fetus’s only source of nourishment, this can cause babies to grow poorly, a condition called intrauterine growth restriction (IUGR).
If a baby is not growing well or if the disease puts the mother’s life in danger, doctors may decide that preterm delivery is the safest approach. If there is time and the baby will be very early, doctors may administer steroids to the mother to speed the baby’s lung development, or magnesium sulfate to prevent eclampsia in the mother and to help prevent cerebral palsy.
The best way to keep you and your baby healthy throughout your pregnancy is to go to all your scheduled prenatal visits so your doctor can check your blood pressure and any other signs and symptoms of preeclampsia.
Most women still can deliver a healthy baby if preeclampsia is detected early and treated with regular prenatal care.
Throughout your pregnancy, your doctor will check:
- Your blood pressure
- Your blood
- Levels of protein in your urine
- How your baby is growing and gaining weight
How Is Preeclampsia Treated?
If you develop mild preeclampsia, your doctor may want you to be less active. In certain cases you may need medication, bed rest, or hospitalization, especially if you have severe preeclampsia.
If you have signs of severe or worsening preeclampsia, you may require observation or treatment in a hospital setting. You will be monitored for signs of HELLP syndrome or eclampsia, and your baby’s health and growth will be monitored.
Medical treatments for preeclampsia can only address the symptoms, not the disorder itself, and include medicines to lower blood pressure and magnesium sulfate to prevent seizures. Your doctor may prescribe blood pressure medicine for you to take at home, but magnesium sulfate must be given in the hospital.
Delivery. The only way to stop preeclampsia entirely, though, is to have your baby. Even then, the condition may develop shortly after delivery and/or persist for up to six weeks. To keep you both healthy, your doctor may want to induce labor so you have your baby earlier than your due date. You may need medication to lower your blood pressure when you deliver.
Depending upon how healthy you and your baby are, your doctor may want you to have a cesarean instead of vaginal delivery.
After delivery. Preeclampsia may require that you to stay in the hospital longer after you give birth. Your blood pressure should return to a normal level a few weeks after you deliver. And preeclampsia usually doesn’t increase your risk for high blood pressure in the future.
How Can I Prevent Preeclampsia?
Unfortunately, there is no way to prevent 100% of cases of preeclampsia. Studies have shown that calcium supplementation or low-dose aspirin may help some women in specific circumstances, but not enough to recommend them for all pregnant women.
Leading a healthy lifestyle can help you to reduce your risk for preeclampsia.
- Use little or no added salt in your meals.
- Drink 6-8 glasses of water a day.
- Don’t eat a lot of fried foods and junk food.
- Get enough rest.
- Exercise regularly.
- Elevate your feet several times during the day.
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. The purpose of this website is to promote broad consumer understanding and knowledge of various health topics. It is not intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition or treatment and before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Resources: https://www.verywellfamily.com/faqs-about-preeclampsia-2748465