Second Trimester Must-Haves
Pregnancy brings a new meaning to the concept of beauty. It is a period of immense joy coupled with excitement. The feeling of carrying a little soul within you is magnificent. Pregnancy is a time to celebrate because a little angel is coming soon.
The second trimester is the best part of pregnancy. Your nausea has subsided, you’re sleeping a little better, plus you’re finally looking legitimately pregnant. You will still probably use some of the things off of my first-trimester must-haves, but below are the list of additional must-haves for a happy second trimester!
Maternity wear
Clothes are definitely getting tighter at this point of your pregnancy so you’ll want to invest in some new clothing. I recommend loose dresses because not only are they comfortable, but they can grow with you and be worn after you have a baby. As your baby belly grows you’ll need a few key items of maternity wear. A good pair of maternity jeans that make you feel comfortable and will last you through the pregnancy is a savvy buy.
Sleep Aids
By now you may need some extra help getting a good night’s sleep. Fans, noise machines, earplugs, and body pillows are all useful aids for helping pregnant women get their zzz’s.
Comfy Pajamas
It’s common to feel really tired while pregnant. Your body is going through so much and working hard so you definitely want to get as much sleep/rest while you can and you will be most comfortable sleeping on your side as your belly grows. Now that your old pajamas probably don’t exactly fit so well anymore, it’s time to get a few pairs of comfortable Pajamas to survive these last few months.
Support Bra
By this stage – if not before – your breasts may have grown and felt more sensitive.Traditional bras don’t have room for the diaphragm to grow during pregnancy and they also have a traditional underwire which is not recommended to wear while pregnant or nursing. Having wider straps on a maternity bra is also important for support, especially for larger cup bras.Maternity bras provide firm elastic support without using wires.
Doula
A doula is a professional trained in childbirth who provides emotional, physical, and educational support to a mother who is expecting, is experiencing labor, or has recently given birth. The doula’s purpose is to help women have a safe, memorable, and empowering birthing experience. Whether you want a natural birth, a medicated birth, or a c-section, a doula is a great person to add to your support team to help you have the positive experience that you want.This is the time during your pregnancy to start interviewing and choosing the right doula for you.
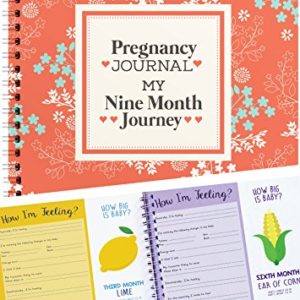
Pregnancy books
Reading is one of the most vital talents a child needs in order to be successful in life. Books are one’s best friend and the early we inculcate this habit, it is excellent for the child. Reading while pregnancy not only increases the knowledge but also helps in making the bond between the mother and the baby stronger. It also triggers better concentration, a good attention span, distressing the mother of her tensions, resulting in a smarter baby.
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. The purpose of this website is to promote broad consumer understanding and knowledge of various health topics. It is not intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition or treatment and before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Resources:
https://www.baby-chick.com/second-trimester-must-haves/
https://www.babycenter.com/0_pregnancy-shopping-checklist-second-trimester_5679.bc