Third Trimester Must-Haves
The final trimester of pregnancy is an exhausting but exciting time!
You’re in your third trimester! Can you believe it? Hopefully, everything has been going smoothly and now you’re finally at the point where you’re preparing for the last few months and getting ready for labor. So exciting! I will say, a lot of women describe the third trimester as the longest trimester since you are getting more uncomfortable by the day and you are so ready to have your body back and meet your baby. You’re almost there though!
Listed below are my must-haves that every woman should have to help her have the best and most enjoyable third trimester.
- Comfy Shoes
With each passing day, your baby is getting bigger. Before you know it, it will feel like you are carrying a bowling ball with you everywhere you go. At this point, the extra weight is getting harder on your feet so getting some comfortable shoes are an absolute MUST! You’ll want to get a pair of flats, sandals, or comfortable sneakers (or all of them) that you can easily slip on and off to make standing and walking throughout the day a bit more bearable.
- Birth Ball
A birth ball is wonderful to have because it strengthens your legs, back, and core muscles — which can condition the abdominal area involved in childbirth — and it can aid in relaxation, comfort, and physical relief. A birth ball is good for exercising the deep, supportive muscles in the lower back and surrounding spine so you’ll have better posture and be less prone to a backache and sciatica. What’s also great is that you can use it during labor and even after when you have your baby. Being able to bounce on it to soothe your crying baby and save your joints at the same time is awesome.
- Heating Pad
Your back and hips will be a lot more aches and sore towards the end of your pregnancy. When you can’t get a Massage or see a chiropractor, remember that heat is your friend. You can heat a rice bag or use a heating pad before you go to bed to help give you relief and relax your muscles.
NOTE: Make sure that you turn off the heating pad before you go to sleep to avoid overheating and burning your skin. Also, heat is a wonderful thing to help you during labor, too. Bring these things in your hospital bag.
- Maternity Leggings
The clothing gods heard our prayers and miraculously made comfy, stretchy leggings a chic wardrobe choice you can practically wear anytime, anywhere. If pregnancy has led to varicose veins and swollen ankles, these maternity compression leggings may be just the thing to offer some relief.
- Loose Tops
Nothing more comfortable than a loose top. A stretchy tee shirt is long enough to cover not only the bump but also the bum- which is tres important when you live in leggings!
- Body Pillow
C-shape pillow cradles you from head to toe, even taking the place of your regular pillow. One end is for your head and neck; the other tucks between your legs to realign your hips as you sleep. A body pillow is a great help in getting best sleep during the 3rd trimester.
- Water Bottle
It’s important to keep hydrated during this stage of pregnancy. Staying hydrated is paramount to your comfort and health. Invest in a giant bottle/cup so that you don’t have to keep getting up and refilling your water bottle. If plain water is getting too boring, switch it up with coconut water, sparkling water, or add a bit of juice.
- Raspberry Leaf Tea
Raspberry Leaf Tea is highly recommended to start drinking during your third trimester every day to help prepare your body for labor and delivery. It’s great for uterine health and helps prevent post-delivery hemorrhaging.
- Books and Resources
It’s time to move on from the pregnancy/delivery books and start looking at resources on actually taking care of a newborn baby. There are lots of great books that have good tips and advice for baby’s feeding, sleeping, and overall scheduling. Watch TV shows and get new ways on how to soothe your baby – every new parent needs to know those tricks. They really talk about the science behind it all.
- Postpartum Doula
So many expecting couples are focusing on the labor and birth of their baby (and rightfully so, it’s very important), but they forget to think about what happens after giving birth – taking care of a baby. Start looking into postpartum doulas in your area. They can help you with breastfeeding, pumping, bottle-feeding, showing you had to soothe, swaddle, all types of newborn care, and so much more. Whether you want help during the day or at night, a postpartum doula is an amazing support person and resource.
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. The purpose of this website is to promote broad consumer understanding and knowledge of various health topics. It is not intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition or treatment and before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
3 Important Exercises during 3rd Trimester
Even though you may not feel like doing much at all as your belly grows week after week, it’s important to keep moving throughout pregnancy, including in the awkward and uncomfortable last weeks. Third-trimester exercises are some of the most important, helping to alleviate aches and pains while also preparing your body for labor. These exercises will open up the hips and pelvis, strengthening the muscles you’ll be using during childbirth.
“Don’t let fatigue rule the end of your pregnancy. Keep up your exercise schedule with this easy-to-follow plan for months 8-9 of your pregnancy.”
Pelvic Floor Exercises 
Pelvic floor exercises help to strengthen the muscles of the pelvic floor. These muscles come under great strain during pregnancy and childbirth.
The pelvic floor muscles are overstretched and weakened underneath that weight so it is important to do pelvic floor exercises to maintain muscle tone. If your pelvic floor muscles are weakened, you may find that you leak urine when you cough, sneeze or strain. This is quite common and you needn’t feel embarrassed. It’s known as stress incontinence and it can continue after pregnancy.
Squats
 The full squat position is a passive position that allows gravity to open the pelvis, causing the pelvic floor muscles to engage. Use a prop if you need to, placing a rolled-up towel or yoga mat under your heels if they don’t reach the ground.
The full squat position is a passive position that allows gravity to open the pelvis, causing the pelvic floor muscles to engage. Use a prop if you need to, placing a rolled-up towel or yoga mat under your heels if they don’t reach the ground.
Squatting can open your pelvic outlet by 10 percent. When you squat to induce labor, it creates more room for the baby to move down into the birth canal. Squatting during the third trimester helps strengthen your leg muscles. Strong legs are a must when it comes to labor and the final push to give birth. It eases constipation and pressure on the pelvic floor – a blessing during the last few weeks of your pregnancy.
Caution:
Though squatting to induce labor is harmless in most cases, but you need to keep some points in mind. If your baby is in breach position, squatting can prove to be harmful. This is because squatting will force her to descend the birth canal without giving her the chance to move into proper position. So talk to your doctor to make sure your baby is head down before you try squatting.
Gentle Abs 
Given all the stretching that your ab muscles go through during pregnancy to accommodate your growing baby, you wouldn’t be the first woman to wonder if there must be something you can do to keep them in shape and speed recovery after birth. And while pregnancy isn’t the time to strive for the chiseled core you’ve always dreamed of, you can certainly take a few safe steps, with the guidance of your practitioner, to maintain your fitness and keep your core strong during pregnancy. In fact, exercising your abs during pregnancy has lots of benefits, including reduced risk for back pain and potentially even a speedier labor.
You can do abdominal exercise in the late stages of pregnancy, as long as they are gentle exercises that don’t over-strain the abdominal muscles. A basic pelvic tilt is a great place to start and is safe at all stages. For more of a challenge, you can add movement to the pelvic tilt by incorporating knee lifts and toe taps.
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. The purpose of this website is to promote broad consumer understanding and knowledge of various health topics. It is not intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition or treatment and before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Resources:
http://www.momjunction.com/articles/benefits-of-doing-squats-to-induce-labor_00113886/#gref
https://www.pregnancybirthbaby.org.au/pelvic-floor-exercises
8 Natural Ways to Induce Labor
As you’re approaching your due date, you’re becoming more and more ready and anxious to meet your little one. Your back is aching, your feet are sore, you can’t sleep comfortably, and most of all you’re so excited to finally see the sweet little face you’ve been dreaming about in person.
Your due date is an educated guess for when your baby might make its arrival. While many women deliver perfectly healthy babies two weeks before or after this presumed due date, it’s recommended that women wait until 40 weeks for delivery. It’s best to let mother nature decide when your baby comes.
Be aware: Any type of labor induction increases the risk of cesarean delivery and other emergency interventions. Always talk to your doctor before trying to induce labor on your own.
8 things that you can do yourself to naturally induce labor
- Nipple Stimulation
Nipple stimulation is one of the most reliable options. It helps release the hormone called oxytocin which is the hormone that causes your uterus to contract. (Oxytocin is also called the love hormone since it’s released when you feel in love.) Oxytocin is the hormone that causes the uterus to contract and milk to be ejected from the breast. In fact, if you choose to breastfeed your baby right after delivery, this same stimulation is what will help your uterus shrink back to its original size. You or your partner may manually stimulate your nipples, or you can try using a breast pump.
- Exercise/ Cardio/ Stair Climbing / Squats
Use gravity to your advantage. Get up and start moving! Physical activity helps move your baby’s head down lower in your pelvis and that allows your baby’s head to put pressure on your cervix which helps it dilate. Try walking for 30 minutes every day. If you can walk up a steep hill, even better! This causes you to lean forward at an angle helping the baby move in the right direction. Walking stairs and doing squats have also been said to be very helpful. So go ahead and get that heart pumping!
Theoretically, there are multiple reasons why having sex could induce labor. For example, sex can release oxytocin, which may help jumpstart uterine contractions. Having sex is safe at full term, but you shouldn’t have sex after your water has broken. Doing so can increase your risk of infection. Pretty much everyone knows or has been told that having sex is the way to start labor. The reason for that is the act of sex can cause contractions. Not only that, semen contains a substance called prostaglandins which helps the cervix to ripen and efface so it’s best that he also orgasms. This prepares your body for labor.
- Acupuncture & Acupressure
Acupuncture stimulates the release of oxytocin in the body. Acupuncture and acupressure is another natural method for inducing labor. With acupuncture, a practitioner places fine needles at various points along the body to balance your energy flow. Acupressure is the same concept, but instead, fingers are used to apply pressure to pressure points. These are also pressed during labor induction massages. A couple of pressure points are thought to cause contractions. One is located in the webbing between your thumb and forefinger. The other is located just above your ankle. Applying pressure to either of these two pressure points may help bring on contractions.
- Red Raspberry Leaf Tea
 Drinking this tea regularly can strengthen and tone your uterus and help those muscles in your uterus start to contract. Midwives often recommend drinking red raspberry leaf tea as your due date nears. Tea may tone and strengthen the uterus in preparation for labor. Even if it doesn’t work, you’ll stay hydrated.
Drinking this tea regularly can strengthen and tone your uterus and help those muscles in your uterus start to contract. Midwives often recommend drinking red raspberry leaf tea as your due date nears. Tea may tone and strengthen the uterus in preparation for labor. Even if it doesn’t work, you’ll stay hydrated.
Soaking in a warm bath may help to get labor going. The reason why? Soaking in the tub helps to relax you. There is evidence that stress and being uptight may keep you from going into labor. This is why massage is also beneficial. Almost anything that gets your mind off of the fact that you are still pregnant that can get you to relax can help.
- Membrane Stripping
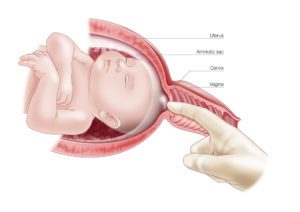 Some providers will offer to strip your membranes to encourage labor. Though the procedure is done in the office, there are no medications involved. Your doctor will use a gloved finger to separate the amniotic sac from the area around the cervix. This action releases hormones called prostaglandins, which help the body go into labor. This one can be quite uncomfortable. It hasn’t been proven to be one of the most effective forms of induction, but it is an option. If you have any vaginal infections, membrane stripping is not an option.
Some providers will offer to strip your membranes to encourage labor. Though the procedure is done in the office, there are no medications involved. Your doctor will use a gloved finger to separate the amniotic sac from the area around the cervix. This action releases hormones called prostaglandins, which help the body go into labor. This one can be quite uncomfortable. It hasn’t been proven to be one of the most effective forms of induction, but it is an option. If you have any vaginal infections, membrane stripping is not an option.
Getting a labor induction massage is a great way to get contractions going. This massage doesn’t always work immediately and may require two or three appointments to help stimulate labor. It allows you to relax your muscles around the baby and it sends signals to your body to start the labor process.
The Waiting Game
Before trying anything that might induce labor, you’ll want to speak with your doctor to go over any risks or possible complications. Though some of these methods are popular folklore among pregnant women, little scientific evidence supports their efficacy. In most cases, it’s best to let baby set their own birth date, even if it means waiting another week or two.
As the due date approaches, many couples are eager for labor to begin so they can finally meet their little one.
And though that’s the most exciting moment of your life, you might want to slow down and not rush through things. Saving your energy, rather than wearing yourself out with schemes for starting labor sooner. In other words, get some sleep while you can!
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. The purpose of this website is to promote broad consumer understanding and knowledge of various health topics. It is not intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition or treatment and before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Resources:
https://www.healthline.com/health/pregnancy/natural-ways-to-induce-labor#takeaway
High-Risk Pregnancy
A pregnancy is considered high-risk when there are potential complications that could affect the mother, the baby, or both. High-risk pregnancies require management by a specialist to help ensure the best outcome for the mother and baby.
If you’re being treated for a lifelong (chronic) condition, you may have known for a long time that becoming pregnant carries additional risks. Or you may find out you have a high-risk pregnancy because of a problem that develops for the first time during pregnancy. having a high-risk pregnancy means it’s more likely that you or your baby will have health problems during pregnancy, birth, or after delivery. These could be minor problems, but in some cases, a high-risk condition can be life-threatening for a woman or her baby. 
Risk Factors for High-Risk Pregnancy
Reasons that a pregnancy may be considered high risk include:
- Blood disorders. If you have a blood disorder, such as sickle cell disease or thalassemia, the additional strain pregnancy puts on your body can make your condition worse. There are also potential risks to your baby (both during pregnancy and after delivery) if she inherits your condition.
- Chronic kidney disease. This condition increases your risk of miscarriage, developing high blood pressure and preeclampsia, and having your baby early. Pregnancy can also put an extra strain on your kidneys.
- HIV or AIDS. If you have HIV or AIDS, your baby can become infected before birth, during delivery, or when you breastfeed. Fortunately, medication can dramatically reduce this risk.
- Lupus. Lupus and other autoimmune diseases can increase your risk of preterm delivery, preeclampsia, and have a small baby. Being pregnant may also increase the likelihood of your disease flaring up or getting worse.
- Maternal age. Your age can affect how likely you are to have a high-risk pregnancy. Being an older mom (age 35 or older in your first pregnancy) or a younger one (in your teens) puts you at greater risk of some complications and health problems.
- Obesity. Having a body mass index (BMI) of 30 or higher before pregnancy puts you at greater risk of gestational diabetes, type 2 diabetes, and high blood pressure during your pregnancy. When it comes to giving birth, you’re more likely to need your labor induced or a cesarean delivery.

- Thyroid disease. Both an underactive thyroid (hypothyroidism) and an overactive thyroid (hyperthyroidism) during pregnancy can cause problems for you and your baby if the condition isn’t controlled. These problems can include miscarriage, preeclampsia, low birth weight, and having your baby early.
- Type 1 or type 2 diabetes. If your diabetes isn’t managed well, you could be at risk of complications including birth defects, high blood pressure, having your baby early, and having a very big baby. Your baby may have problems with breathing, low glucose levels, and jaundice.
Pregnancy-related issues:
Often a pregnancy is classified as high risk because of issues that arise from the pregnancy itself and that have little to do with the mother’s health. These include:
- Premature Labor is also called preterm labor. It’s when your body starts getting ready for birth too early in your pregnancy. Labor is premature if it starts more than three weeks before your due date. Many factors have been associated with an increased risk of preterm labor, however, including Previous preterm labor or premature birth, particularly in the most recent pregnancy or in more than one previous pregnancy. Pregnancy with twins, triplets or other multiples. Problems with the uterus, cervix or placenta
- Multiple births mean you are carrying more than one baby (twins, triplets, quadruplets, etc.). Multiple pregnancies, which are more common as women are using more infertility treatments, increase the risk of premature labor, gestational diabetes, and pregnancy-induced high blood pressure.
- Placenta Previa is a problem of pregnancy in which the placenta grows in the lowest part of the womb (uterus) and covers all or part of the opening to the cervix. The placenta grows during pregnancy and feeds the developing baby. If the placenta still covers the cervix close to delivery, the doctor may schedule a cesarean section to reduce bleeding risks to the mother and baby.
- Fetal problems, which can sometimes be seen on ultrasound. Approximately 2% to 3% of all babies have a minor or major structural problem in development. Sometimes there may be a family history of fetal problems, but other times these problems are completely unexpected.
How does being high-risk affect my labor?
It’s worth preparing yourself for the idea that the birth you have may not be the birth you’d choose. If your pregnancy is high-risk, you won’t have the option of a home birth or attending a birth center. You’ll need to give birth in a hospital where you and your baby can be monitored closely and specialist care is available during the birth and afterward.
If you’re having multiples, you’re more likely to go into labor early. Preterm labor is also more likely if you have a high-risk pregnancy for other reasons, such as having too much amniotic fluid around the baby or having certain medical conditions. You may also need to have your labor induced to prevent or reduce health problems for you and your baby. Or there may be reasons why a vaginal birth isn’t possible and you need to have a cesarean section.
Talk to your provider about what you can expect during labor, so you can prepare yourself in the best way possible.
Will my baby be okay if I’m high-risk?
 If you have a high-risk pregnancy, one of your biggest worries will probably be whether any harm will come to your baby. It’s natural to be concerned. However, with good prenatal care, it’s possible to have a healthy baby. Healthy moms grow healthy babies: Some conditions, as well as the drugs that are usually prescribed to manage them, pose a risk to your baby’s health. But stopping medications that you take for a condition can also be very dangerous.
If you have a high-risk pregnancy, one of your biggest worries will probably be whether any harm will come to your baby. It’s natural to be concerned. However, with good prenatal care, it’s possible to have a healthy baby. Healthy moms grow healthy babies: Some conditions, as well as the drugs that are usually prescribed to manage them, pose a risk to your baby’s health. But stopping medications that you take for a condition can also be very dangerous.
If your baby is born early, he could have difficulty breathing or feeding, or develop infections or other complications. If this happens, he needs extra care and support, which means staying in the hospital for several weeks, probably in a Neonatal Intensive Care Unit (NICU).
How can I reduce the risk of pregnancy complications?
Find out all you can about your condition and what you can do to stay healthy. Ask your provider for information. At your first prenatal visit, tell your provider about any current health problems you have, any medication you’re taking, and any difficulties you had in previous pregnancies. Have a healthy lifestyle: Follow your provider’s nutritional guidance, gain the right amount of weight, and stay active if you’re able. Don’t smoke or drink alcohol.
Ask your partner, family, and friends for support – this is likely to be a stressful time. Look after your emotional well-being. Take time out for yourself and reduce your stress levels where you can.
If your pregnancy is considered high risk, your doctor may refer you to a perinatologist. Also called a maternal-fetal medicine specialist, a perinatologist is an Obstetrician with special training in high-risk pregnancy care. This specialist will work with your other doctors, nurses, and other health-care professionals to ensure the best possible outcome for both you and your baby.
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. The purpose of this website is to promote broad consumer understanding and knowledge of various health topics. It is not intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition or treatment and before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Resources:
https://www.webmd.com/baby/managing-a-high-risk-pregnancy#1
Does “Pregnancy Brain” Exist?
Pregnancy brain typically refers to lapses in attention and memory. About 80 percent of new mothers report difficulties remembering things that once came naturally, and although not all studies support this, the weight of the evidence shows that during pregnancy, women exhibit measurable declines in important cognitive skills.
Pregnant women are also better at recognizing fear, anger, and disgust. This enhanced ability to identify and discriminate among emotions may help mothers to ensure their infants’ survival. Research from my laboratory has shown that the hormone exposures in pregnancy—for example, high levels of estrogens and oxytocin—are associated with heightened maternal responsiveness and sensitivity to the environment and infants’ needs.
“Relax, pregnancy does not change your brain. But it may affect how mentally sharp you feel.”
Pregnancy Brain a Myth or a Reality?
Fortunately (or unfortunately, depending on how you look at it), there’s no scientific research that proves you get flakey during pregnancy. But even if “pregnancy brain” is just a myth, there are still tons of women who complain of feeling more forgetful or spaced out during their pregnancy.
Pregnancy does not change a woman’s brain even though some women don’t feel as sharp as usual when they’re pregnant.
What Causes “Momnesia?”
If you’re experiencing memory lapses or periods of forgetfulness, chances are your fellow moms-to-be can relate. So what’s to blame? Hormonal changes, lack of sleep, and/or the distractions of spending a lot of time thinking (and stressing) about the baby are the likely causes. Surging hormone levels and new priorities may help explain why pregnancy brain happens.
What Pregnancy Brain Feels Like
Pregnancy brain is “the feeling of walking into a room, going after something, and not remembering what you went for about five to 10 times a day. Many pregnant women and new moms spend a lot of time thinking about the changes that having a baby will bring or taking care of their newborn. As a result, their short-term memory may suffer.
How to Help Your Memory
After the baby arrives, sleep deprivation is clearly a contributing factor. Brizendine says, “Women accumulate up to 700 hours of sleep debt in the first year after having a baby and that causes the brain not to be at its best for things other than caring for the baby.”
Save your sanity by writing things down and making lists, along with snacking regularly and getting lots of rest. Also, be sure to take your prenatal vitamins —they contain ingredients that help boost mental sharpness. Don’t worry, it’s annoying, but it isn’t permanent.
Pregnancy primes the brain for dramatic neuroplasticity, which is further stimulated by delivery, lactation and mother-child interactions. Some evolutionary biologists have argued that the development of maternal behaviors is the primary force shaping the evolution of the mammalian brain. Of interest, these alterations may become more pronounced with each successive pregnancy and persist throughout a mother’s lifespan. But helpful adaptations are rarely achieved without an associated cost—and pregnancy brain may reflect just such a cost.
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. The purpose of this website is to promote broad consumer understanding and knowledge of various health topics. It is not intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition or treatment and before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Resources:
https://www.webmd.com/baby/features/memory_lapse_it_may_be_pregnancy_brain#1
Importance of Genetic Testing Before & During Pregnancy
All soon-to-be parents want their children to be healthy and to have a pregnancy free of major complications. Unfortunately, complications can occur during pregnancy, either with the mother’s health or the child’s. Sometimes, the mother and child are at risk for certain complications throughout the pregnancy because of their family history and genetics.
 All pregnant women are offered some form of testing for genetic problems. Now, deciding whether you want to have it done is completely personal. You will want to weigh different factors, including baby’s risk for genetic problems.
All pregnant women are offered some form of testing for genetic problems. Now, deciding whether you want to have it done is completely personal. You will want to weigh different factors, including baby’s risk for genetic problems.
What is genetic testing (carrier screening)?
Carrier testing is a type of genetic testing that is used to determine if a person is a carrier for a specific autosomal recessive disease. This kind of testing is used most often by couples who are considering becoming pregnant to determine the risks of their child inheriting one of these genetic disorders. In other words, if you screen positive for a genetic abnormality but your partner does not, your child will not inherit the condition. And even if you both screen positive, there’s only a 25 percent chance your baby will have the disease.
When should you get genetic testing?
Getting screened before you try to get pregnant can give you reassurance (if you or your partner is not a carrier, it’s one less thing to worry about when do you get pregnant) or can help you make an informed game plan for pregnancy. If it turns out that you are both carriers, you can be prepared for and bone up on what it means to have a baby with the genetic condition, choose to learn about certain prenatal tests to check whether your baby’s healthy, or you can consider other options like egg or sperm donation or adoption.
Getting tested once you become pregnant (if you hadn’t done so ahead of time) can help you and your doctor decides the right prenatal tests for your baby, and what to look for if you choose to have them. If you know that your baby’s at an increased risk for having cystic fibrosis or sickle cell disease, for instance, your doctor can look for those conditions specifically through either a CVS (chorionic villi sampling) or amniocentesis.
Who are genetic carriers?
If both partners in a couple carry the same recessive disease, then the couple have a one in four chance of a child with that disease. Carrier couples may, therefore, have multiple affected children. Some recessive diseases are relatively mild but others are severe, including many that cause death at or shortly after birth.
What are some of the most common genetic diseases? 
- Cystic fibrosis is a life-threatening condition that causes lung damage and digestive problems. It is a progressive, genetic disease that causes persistent lung infections and limits the ability to breathe over time. In people with CF, a defective gene causes a thick, sticky buildup of mucus in the lungs, pancreas, and other organs.
- Sickle cell disease is a disorder of the blood caused by an inherited abnormal hemoglobin (the oxygen-carrying protein within the red blood cells). The abnormal hemoglobin causes distorted (sickled) red blood cells. The sickled red blood cells are fragile and prone to rupture, most common in people of African and Mediterranean backgrounds, cause a blood disorder that leads to anemia, a weakened immune system, and other health complications.
- Thalassemia is another blood disorder common to people of African and Mediterranean descent. It is an inherited blood disorder in which the body makes an abnormal form of hemoglobin. Hemoglobin is the protein molecule in red blood cells that carries oxygen. The disorder results in excessive destruction of red blood cells, which leads to anemia and bone growth and liver problems; in severe cases, some babies born with the condition may not survive.
- Tay-Sachs Disease, which mainly affects people of French Canadian and Eastern European Jewish descent, is a disorder of the central nervous system that’s usually fatal in early childhood. Eastern European Jews also face an increased risk for another nervous system disorder called Canavan disease as well as a number of other conditions including familial dysautonomia, familial hyperinsulinism, and Gaucher disease. Your doctor can screen for all of these conditions at the same time.
- Fragile X Syndrome is a genetic condition that causes a range of developmental problems including learning disabilities and cognitive impairment and mental retardation. Usually, males are more severely affected by this disorder than females. Affected individuals usually have delayed development of speech and language by age 2. It is not linked to a specific ethnic background. Reviewing your family’s health history with a doctor or genetic counselor may help you decide whether you should be screened for Fragile X.
Benefits
 When pre-pregnancy carrier screening programs are introduced, they reduce death and disease associated with screened diseases. They can save families from experiencing the tragedy of a child affected by a significant genetic disease. They also reduce the burden of recessive disease with the population as a whole. Each recessive disease is rare but there are hundreds of recessive diseases and so collectively they have wide-ranging social and economic impacts.
When pre-pregnancy carrier screening programs are introduced, they reduce death and disease associated with screened diseases. They can save families from experiencing the tragedy of a child affected by a significant genetic disease. They also reduce the burden of recessive disease with the population as a whole. Each recessive disease is rare but there are hundreds of recessive diseases and so collectively they have wide-ranging social and economic impacts.
So pre-pregnancy carrier screening programs that include many genetic diseases, as now recommended by the American College, would maximize knowledge of genetic risk for couples.
Limitations
When testing genes, some identified variations are definitely harmful while most are definitely harmless. But for some variations, we can’t be sure if they are harmful, and whether or not they will cause disease in any children. There is no guarantee that pre-pregnancy screening will result in a healthy baby, but it will allow couples options to reduce the burden of disease associated with known disease-causing mutations.
Counseling is required before and after the test to explain the risks to couples.
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. The purpose of this website is to promote broad consumer understanding and knowledge of various health topics. It is not intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition or treatment and before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Resources:










