10 Common Pregnancy Myths & Facts
It goes without saying that pregnancy is an exciting and equally confusing time. With just about everyone you know introducing you to new supposed truths about pregnancy, it is common for you to get lost and not know what to believe. While most myths about pregnancy cannot be backed up with facts, a few of them may be worth your consideration.
Common Myths about Pregnancy You Should Be Aware of
- Myth: Pregnant women should not take a bath too often.
Pregnant women are often advised not to bathe regularly.
Fact: This myth has absolutely no foundation at all. Bathing keeps you clean and free of germs that may harm your baby. It is a good hygiene practice and should be followed during pregnancy just as you would follow it on other days.
However, do not take very hot showers as it could raise your body temperature and lead to developmental problems in the baby. As a general rule, avoid bathing in water hot enough to raise your body temperature over 102.2 degrees Fahrenheit. Water temperature of 98.6 degrees Fahrenheit is considered safe for pregnant women.
It is believed that if your belly is lying low then you will have a boy and you will have a girl if your belly is lying high. It is also said that a fast fetal heart rate indicates a girl and a slow fetal heart rate indicates a boy.
Fact: The elevation of the belly is entirely dependent on various physiological factors of the woman. Actually, stomach muscles stretch with subsequent pregnancies. So, if a woman’s belly is higher up, it probably just means she has strong abdominal muscles or it’s her first pregnancy.
A popular notion present in most societies that you will be eating for two when you get pregnant.
Fact: A pregnant woman only needs to add a portion of extra calories to support the baby and not have meals that are made for two people. The exact quantity of calories depends on the weight, height, level of activity of the women, as well as the trimester of pregnancy. On average, women need to consume about 300 additional calories during pregnancy.
Some believe that drinking an occasional glass of wine is harmless during pregnancy and can have no bearing on your baby.
Fact: Alcohol should be avoided at all costs during pregnancy. This is because there has been no study about the quantity of alcohol that is considered safe when you are pregnant. A mother who has consumed alcohol during pregnancy may put her baby at risk of FASD (Foetal Alcohol Spectrum Disorder). Babies of mothers who’ve consumed alcohol also have a higher chance of having congenital disabilities, brain, and cell damage.
- Myth: You Shouldn’t Have Sex During Pregnancy
It is believed that sex during pregnancy can cause miscarriage or may even induce labour.
Fact: Sex does not induce labour. It is completely safe to engage in intercourse with your partner during pregnancy provided it is done in a position that does not put a lot of pressure on your tummy. Your baby is within an amniotic sac that keeps it well-protected. In addition to this, your cervix also has a mucous plug to help guard your baby against infections. Prostaglandins, substances in semen, plus the contractions that occur during sex, can hasten labor in some cases. Some doctors even prescribe it.
However, doctors may advise you against it if you have complications like placenta praevia, a dilated cervix, cervical insufficiency, ruptured membranes, abnormal discharge, and if you are at the risk of premature labour.
- Myth: Pregnant Women Shouldn’t Exercise
Exercising while pregnant can harm the baby and cause miscarriage or induce premature labour.
Fact: Moderate walking or swimming are excellent ways to stay healthy. It may also help you prepare for the delivery. Doctors often advise women to engage in moderate exercises for the same reason. However, it is important not to overwork yourself and seek permission from your doctor before engaging in any exercise.
- Myth: Eating Spicy Food Can Induce Labour and causes blindness in babies.
It is believed that eating hot and spicy foods can lead to miscarriage and induce labour.
Fact: There is no evidence to support this myth. The only disadvantage of eating spicy food is the heartburn and gas that you may have to suffer through later. If you include a moderate quantity of spicy food in your diet during pregnancy, it will do you no harm. Medical experts agree that spicy foods are safe to consume during pregnancy. Spicy foods will not harm your growing baby and might even help your baby develop a taste for certain spices later in life. Although most spicy dishes are safe to eat during pregnancy, avoid dishes that contain undercooked meat, poultry or seafood; unpasteurized dairy products; and fish with high traces of mercury, including swordfish, shark, and mackerel. If you are eating out, ask the waiter about dishes to ensure your dish does not include these foods, which have been known to cause birth defects.
- Myth: You Cannot Take Flights While Pregnant
Flying during pregnancy isn’t safe for the baby due to the radiation in the airport scanners and due to the long duration of some flights.
Fact: It is true that long flights (over 5 hours) may cause problems especially if you are prone to blood clots. Hence, it is best to avoid long flights. However, if you are in good health and have a normal pregnancy, there is no reason why you shouldn’t be flying. Most airlines have restrictions on pregnant women during late pregnancy to prevent labour on the route.
Pregnant women as asked to stay away from cats to prevent getting in contact with parasites.
Fact: While you will not have to stay away from cats, this is partially true. Cat feces contain a virus that may cause toxoplasmosis infection. Hence, it is best not to clean your cat’s litter to avoid exposure to the virus.
- Myth: Your Skin Will Glow During Pregnancy
It is believed that pregnancy makes your skin radiant and gives you an evident natural glow.
Fact: The pregnancy glow myth has some truth to it. During pregnancy, there is increased blood flow in your body, which keeps your skin moisturized and nourished. This, paired with a surge in hormones can contribute to a healthier and brighter looking skin.
However, not every woman is lucky to experience this. Many women also face acne breakouts and other skin problems that may leave their skin looking and feeling worse. The consolation is that most of these conditions rescind after pregnancy.
There’s so much to learn about pregnancy and still many unknowns. If you are pregnant or plan on becoming pregnant, work with your doctor. They can help you come up with a plan for a healthy pregnancy and delivery and can answer any questions you have about symptoms, complications, and what to expect.
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. The purpose of this website is to promote broad consumer understanding and knowledge of various health topics. It is not intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition or treatment and before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Resources: https://www.healthline.com/health/pregnancy/pregnancy-facts
https://www.webmd.com/baby/pregnancy-myths-dos-donts#2
https://www.pregnancybirthbaby.org.au/common-myths-about-pregnancy
What is HELLP Syndrome?
HELLP syndrome is a rare but serious condition that can happen when you’re pregnant or right after you have your baby. There are still many questions about the serious condition of HELLP syndrome. The cause is still unclear to many doctors and often HELLP syndrome is misdiagnosed. It is named for 3 features of the condition:
Hemolysis: This is the breakdown of red blood cells. These cells carry oxygen from your lungs to your body.
Elevated Liver Enzymes: When levels are high, it could mean there’s a problem with your liver.
Low Platelet Count: Platelets help your blood clot.
It is often assumed that HELLP Syndrome will always occur in connection with preeclampsia, but there are times when the symptoms of HELLP will occur without a diagnosis of preeclampsia being made. About 4-12% of women with diagnosed preeclampsia will develop HELLP syndrome. Unfortunately since the symptoms of HELLP syndrome may be the first sign of preeclampsia, this is what can often lead to a misdiagnosed. The symptoms of HELLP may cause misdiagnosed of other conditions such as hepatitis, gallbladder disease, or idiopathic/thrombotic thrombocytopenic purpura (ITP), which is a bleeding disorder.
Cause
The cause of HELLP syndrome is unclear. Although it is more common in women who have preeclampsia or pregnancy induced hypertension (high blood pressure during pregnancy), some women develop HELLP syndrome without showing signs of these conditions.
The following risk factors may increase a woman’s chance to develop HELLP syndrome:
- Having a previous pregnancy with HELLP syndrome
- Having preeclampsia or pregnancy induced hypertension
- Being over age 25
- Being Caucasian
- Multiparous (given birth 2 or more times)
In less than 2 percent of women with HELLP syndrome, the underlying cause appears to be related to LCHAD deficiency in the fetus.
A variety of genetic factors (both in the mother and fetus) have been found to play a role in the development of preeclampsia and HELLP syndrome. However, the condition is likely multifactorial. This means that several genetic and environmental factors likely interact to cause HELLP syndrome, and no one gene is thought to be responsible for the condition.
Some women may have a genetic predisposition to developing preeclampsia and related conditions, such as HELLP syndrome. This means that certain genetic factors increase a woman’s risk to develop HELLP syndrome. However, many women with a genetic predisposition will never develop HELLP syndrome.
Symptoms
The most common symptoms of HELLP syndrome include:
- Headaches
- Nausea and vomiting that continue to get worse–(This may also feel like a serious case of the flu).
- Upper right abdominal pain or tenderness
- Fatigue or malaise
- Nosebleed
- Seizures
A woman with HELLP may experience other symptoms that often can be attributed to other things such as normal pregnancy concerns or other pregnancy conditions.
- Visual disturbances
- High blood pressure
- Protein in urine
- Edema (swelling)
- Severe headaches
- Bleeding that doesn’t stop as quickly as usual
Diagnosis
If you have symptoms of HELLP syndrome, talk to your doctor. She’ll do a physical exam and tests to check for things like:
- High Blood pressure
- Pain in the upper right side of your belly
- Enlarged Liver
- Swollen legs
- Liver Function
- Blood platelet count
- Bleeding into your liver
Treatments
The main solution for HELLP syndrome is to give birth as soon as possible. This means your baby may have to be born early. The risks are too serious for you and your baby if you stay pregnant with HELLP syndrome.
Treatment may also include:
- Corticosteroid medicine to help your baby’s lungs develop more quickly
- Medicine for high blood pressure
- Meds to prevent seizures
- Blood transfusion
Prevention
There’s no way to prevent HELLP syndrome. Since HELLP syndrome is believed to be related to preeclampsia, staying vigilant about diet, exercise and a healthy blood pressure can only help. The best thing you can do is keep yourself healthy before and during pregnancy and watch for early signs of the condition. The following steps can help:
- See your doctor regularly for prenatal visits.
- Tell your doctor if you’ve had any high-risk pregnancies or someone in your family has had HELLP syndrome, preeclampsia, or other blood pressure problems.
- Know the symptoms and call your doctor ASAP if you have them.
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. The purpose of this website is to promote broad consumer understanding and knowledge of various health topics. It is not intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition or treatment and before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Resources:
https://rarediseases.info.nih.gov/diseases/8528/hellp-syndrome
https://www.webmd.com/women/what-is-hellp-syndrome#1
Preeclampsia: Prevention, Management, and Risks
Preeclampsia is a pregnancy disorder that involves high blood pressure rises higher than 140/90 mm Hg after week 20 of your pregnancy along with other symptoms,You also may be tested for protein in your urine because of stress on your kidneys. Other names for preeclampsia include toxemia, pregnancy-induced hypertension (PIH), and gestosis. Preeclampsia is one of four hypertensive disorders of pregnancy and this condition could seriously hurt you and your baby, if you don’t receive treatment, it can harm your brain, kidneys, and liver. You can also develop eclampsia, which can put both your lives at risk.
It may ease your mind to know you can greatly reduce the risk of preeclampsia by going to all your prenatal appointments. In fact, most pregnant women who have preeclampsia have healthy babies.
Learn why you are at risk and what you can do to have the safest pregnancy possible.
Am I at Increased Risk?
Up to 8% of pregnancies are affected by preeclampsia.
Your risk for developing preeclampsia is greater if you have a history of:
- High blood pressure before pregnancy
- Preeclampsia or high blood pressure during a past pregnancy
- Diabetes or kidney disease
- An autoimmune disorder such as rheumatoid arthritis, scleroderma, or lupus
You are also at increased risk if you:
- Are a teen or older than age 40
- Obesity
- First pregnancy
- Twin/multiple pregnancy
- Donor egg pregnancies
- Family history of preeclampsia
How Does Preeclampsia Affect Pregnant Women?
If preeclampsia is not treated quickly and properly, it can lead to serious complications for the mother such as liver or renal failure and future cardiovascular issues.
Because preeclampsia affects many organ systems in the body, increased blood pressure is only one of many symptoms that may be present. Other symptoms of preeclampsia include increased protein in the urine and generalized swelling.
In some women, preeclampsia becomes very severe. Signs that the condition is worsening should be reported to your doctor immediately and include:
- Reduced urine output
- Trouble with vision
- Abdominal pain
- Headache
- Nausea/vomiting
- Seizures
It may also lead to the following life-threatening conditions:
- Eclampsia– This is a severe form of preeclampsia that leads to seizures in the mother.
- HELLP Syndrome (hemolysis, elevated liver enzymes, and low platelet count)- This is a condition usually occurring late in pregnancy that affects the breakdown of red blood cells, how the blood clots, and liver function for the pregnant woman.
How Does Preeclampsia Affect Babies?
Preeclampsia affects babies primarily by reducing the amount of blood that flows through the placenta. Because the placenta is the fetus’s only source of nourishment, this can cause babies to grow poorly, a condition called intrauterine growth restriction (IUGR).
If a baby is not growing well or if the disease puts the mother’s life in danger, doctors may decide that preterm delivery is the safest approach. If there is time and the baby will be very early, doctors may administer steroids to the mother to speed the baby’s lung development, or magnesium sulfate to prevent eclampsia in the mother and to help prevent cerebral palsy.
The best way to keep you and your baby healthy throughout your pregnancy is to go to all your scheduled prenatal visits so your doctor can check your blood pressure and any other signs and symptoms of preeclampsia.
Most women still can deliver a healthy baby if preeclampsia is detected early and treated with regular prenatal care.
Throughout your pregnancy, your doctor will check:
- Your blood pressure
- Your blood
- Levels of protein in your urine
- How your baby is growing and gaining weight
How Is Preeclampsia Treated?
If you develop mild preeclampsia, your doctor may want you to be less active. In certain cases you may need medication, bed rest, or hospitalization, especially if you have severe preeclampsia.
If you have signs of severe or worsening preeclampsia, you may require observation or treatment in a hospital setting. You will be monitored for signs of HELLP syndrome or eclampsia, and your baby’s health and growth will be monitored.
Medical treatments for preeclampsia can only address the symptoms, not the disorder itself, and include medicines to lower blood pressure and magnesium sulfate to prevent seizures. Your doctor may prescribe blood pressure medicine for you to take at home, but magnesium sulfate must be given in the hospital.
Delivery. The only way to stop preeclampsia entirely, though, is to have your baby. Even then, the condition may develop shortly after delivery and/or persist for up to six weeks. To keep you both healthy, your doctor may want to induce labor so you have your baby earlier than your due date. You may need medication to lower your blood pressure when you deliver.
Depending upon how healthy you and your baby are, your doctor may want you to have a cesarean instead of vaginal delivery.
After delivery. Preeclampsia may require that you to stay in the hospital longer after you give birth. Your blood pressure should return to a normal level a few weeks after you deliver. And preeclampsia usually doesn’t increase your risk for high blood pressure in the future.
How Can I Prevent Preeclampsia?
Unfortunately, there is no way to prevent 100% of cases of preeclampsia. Studies have shown that calcium supplementation or low-dose aspirin may help some women in specific circumstances, but not enough to recommend them for all pregnant women.
Leading a healthy lifestyle can help you to reduce your risk for preeclampsia.
- Use little or no added salt in your meals.
- Drink 6-8 glasses of water a day.
- Don’t eat a lot of fried foods and junk food.
- Get enough rest.
- Exercise regularly.
- Elevate your feet several times during the day.
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. The purpose of this website is to promote broad consumer understanding and knowledge of various health topics. It is not intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition or treatment and before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Resources: https://www.verywellfamily.com/faqs-about-preeclampsia-2748465
Gestational Diabetes and Pregnancy: What you need to know
Gestational diabetes mellitus or GDM is one of the most common diet-related complications during pregnancy. It only happens during pregnancy. It means you have high blood sugar levels, but those levels were normal before you were pregnant.
In gestation, the placenta produces hormones that help the baby to grow and develop. These hormones also block the action of the insulin, which is the hormone that helps to keep glucose (or blood sugar) at normal levels. This is called insulin resistance. Because of this insulin resistance, the need for insulin in pregnancy is 2 or 3 times higher than normal. If the body is unable to produce this much insulin, gestational diabetes develops.
If you have it, you can still have a healthy baby with help from your doctor and by doing simple things to manage your blood sugar, also called blood glucose.
It is most commonly diagnosed around the third trimester (usually around the 24th to 28th week of pregnancy) and in most of the cases goes away once the baby is born. Gestational diabetes makes you more likely to develop type 2 diabetes, but it won’t definitely happen.
WHO ARE AT GREATER RISK?
It affects between 2% and 10% of pregnancies each year. Women who are at greater risk of developing gestational diabetes are:
- Mothers who are over 25 years of age
- Having a family history of type 2 diabetes
- Were overweight before you got pregnant
- Women from certain ethnic backgrounds including Vietnamese, Chinese, middle eastern, Polynesian or Melanesian.
- Women who have had gestational diabetes
- Women who have had large babies or obstetric complications
- Have given birth to a baby that was stillborn or had certain birth defects
- A woman who has had a polycystic ovarian syndrome
Gestational Diabetes Symptoms
Women with gestational diabetes usually have no symptoms. Most learn they have it during routine pregnancy screening tests.
Rarely, especially if the gestational diabetes is out of control, you may notice: 
- Feeling more thirsty
- Feeling more hungry and eating more
- A need to pee more
Gestational Diabetes Treatment
To treat your gestational diabetes, your doctor will ask you to:
- Check your blood sugar levels four or more times a day.
- Do urine tests that check for ketones, which mean that your diabetes is not under control
- A balanced diet is key to properly managing gestational diabetes. In particular, women with gestational diabetes should pay special attention to their carbohydrate, protein, and fat intake.
- Eat a healthy diet that’s in line with your doctor’s recommendations
- Make exercise a habit
Your doctor will track how much weight you gain and let you know if you need to take insulin or other medicine for your gestational diabetes.
Why Is Managing Blood Sugar Especially Important for Pregnant Women With Gestational Diabetes? 
Most women who develop diabetes during pregnancy go on to have a healthy baby. Dietary changes and exercise may be enough to keep blood sugar (glucose) levels under control, though sometimes you may also need to take medication.
But untreated gestational diabetes can cause serious problems. If blood sugar levels remain elevated, too much glucose ends up in the baby’s blood. When that happens, the baby’s pancreas needs to produce more insulin to process the extra sugar.
Too much blood sugar and insulin can make a baby put on extra weight, which is stored as fat. This can make the baby grow very large (macrosomia).
Also, high blood sugar levels during pregnancy and labor increase the risk of a baby developing low blood sugar (hypoglycemia) after delivery. That’s because the baby’s body produces extra insulin in response to the mother’s excess glucose. Insulin lowers the amount of sugar in the blood.
The signs and symptoms of hypoglycemia in an infant include:
- jitteriness
- weak or high-pitched cry
- floppiness
- lethargy or sleepiness
- breathing problems
- skin that looks blue
- trouble feeding
- eye rolling
- Seizures
A baby may also be at higher risk for breathing problems at birth, especially if blood sugar levels aren’t well controlled or the baby is delivered early. (If you have gestational diabetes, your baby’s lungs tend to mature a bit later). The risk of newborn jaundice is higher too.
If your blood sugar control is especially poor, the baby’s heart function could be affected as well, which can contribute to breathing problems. Gestational diabetes sometimes thickens a baby’s heart muscle (hypertrophic cardiomyopathy), causing the baby to breathe rapidly and not be able to get enough oxygen from her blood.
Can gestational diabetes be prevented?
It’s not possible to prevent gestational diabetes entirely. However, adopting healthy habits can reduce your chances of developing the condition. If you’re pregnant and have one of the risk factors for gestational diabetes, try to eat a healthy diet and get regular exercise. Even light activity, such as walking, may be beneficial.
If you’re planning to become pregnant in the near future and you’re overweight, one of the best things you can do is work with your doctor to lose weight. Even losing a small amount of weight can help you reduce your risk of gestational diabetes.
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. The purpose of this website is to promote broad consumer understanding and knowledge of various health topics. It is not intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition or treatment and before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Childbirth Delivery Methods and Types
Every woman’s experience is unique but most mothers would honestly say, yes, childbirth is painful. However, it is short-lived, and there are many types and methods to effectively reduce the intensity of childbirth pain. There are many choices in childbirth. Women can choose the method that makes them most comfortable, and that makes sense for their personal and medical situation.
Medical technology has made childbirth a much safer experience over the past century for both mother and baby. Hospitals have responded to trends in childbirth, such as the need for a more home-like environment in the hospital. Many hospitals now offer comfortable maternity suites that convert into state of the art delivery rooms.
An easy birth and a perfectly executed birth plan are ideal. But we know that even the most carefully planned birth can take twists and turns. In those cases, it’s important to be prepared for alternative delivery methods.
Different Kinds of Childbirth and Delivery Methods
Vaginal Delivery
 In a vaginal birth, the baby is born through the birth canal. It’s hard to know when exactly you will go into labor, but most women give birth at around 38-41 weeks of pregnancy.
In a vaginal birth, the baby is born through the birth canal. It’s hard to know when exactly you will go into labor, but most women give birth at around 38-41 weeks of pregnancy.
A vaginal birth without medication benefits both mother and baby. The microbiome, or bacterial environment, is established by birth method. There is some research that suggests the development of the infant microbiome is associated with the likelihood of developing allergic diseases during childhood, but the association isn’t clear.
Benefits of vaginal delivery:
- Infants born vaginally tend to have fewer respiratory problems.
- Quicker recovery for the mother
- A lower rate of infection and a shorter hospital stay
Disadvantages of vaginal delivery
- Tearing of the perineum
- Sometimes, a vaginal birth may not be recommended for medical reasons.
According to the Centers for Disease Control (CDC), about 1/3 of births are delivery by C-section, although rates are highly variable by hospital and region. The World Health Organization (WHO) says the rate of Cesarean deliveries should be about 10%-15%; the higher level is because of both elective Cesareans and overuse in the U.S.4 A C-section involves a horizontal incision across the lower abdomen through which the infant is delivered. The typical hospital stay is three days after a Cesarean to ensure the incision is healing. Full recovery can take 8 weeks. One advantage of a C-section is that the delivery date can be planned ahead of time. In certain circumstances, a C-section is scheduled in advance. In others, it’s done in response to an unforeseen complication.
Events that may require C-Section:
- Multiples (twins, triplets, etc)
- A very large baby
- Previous surgery, C-Sections, or other uterine conditions
- Baby is in breech (bottom first) or transverse (sideways) position
- Placenta previa (when the placenta is low in the uterus and covers the cervix)
- Fibroid or other large obstruction
- Medical conditions/complications
Water Birth
 A water birth means the mother goes through some or all of the stages of childbirth in a portable tub similar to a hot tub. The baby can be delivered underwater or the mother can get out of the water and deliver in a different position. Women chose water births because it can be more relaxing, and less painful to be in the water. Birthing tubs can be brought into the home for a home birth, and they are often found in birthing centers. Some hospitals may have birthing tubs as well.
A water birth means the mother goes through some or all of the stages of childbirth in a portable tub similar to a hot tub. The baby can be delivered underwater or the mother can get out of the water and deliver in a different position. Women chose water births because it can be more relaxing, and less painful to be in the water. Birthing tubs can be brought into the home for a home birth, and they are often found in birthing centers. Some hospitals may have birthing tubs as well.
Benefits of Water Birth:
- It allows the woman to move into a variety of positions that can feel more natural and less painful.
- The partner can also get into the tub with the mother to support the delivery.
Disadvantages of Water Birth:
- May increase the risk of infection, but as long as the water is fresh and clean, water births are not any riskier than non-water births.
- Unless the water birth takes place in a birth center with established tubs, there are logistics involved in setting up the tub and warming the water for a water birth.
- If the birth plan at home does not progress normally, it may require transport to a hospital.
The Lamaze method is typically known for controlled breathing techniques but it includes a number of comfort strategies that can be used during labor. Breathing techniques increase relaxation and decrease the perception of pain. In addition to breathing, other information about preparing for childbirth is covered. Lamaze is taught in a series of classes attended by both the mother and her partner, when possible. The Lamaze method doesn’t explicitly encourage or discourage medications but seeks to educate women about their options so they can make a birth plan that suits their individual needs.
Benefits of the Lamaze Method:
- Lamaze training prepares the mother and her partner with a number of tools to use to get through labor and delivery naturally.
- The breathing and relaxation techniques reduce the perception of pain and keep labor moving smoothly.
- The Lamaze courses help the couple be prepared with what to expect over the first few days and weeks together.
Disadvantages of the Lamaze Method:
- Learning the Lamaze method takes time. The couple must plan ahead and attend classes starting in the second trimester of pregnancy.
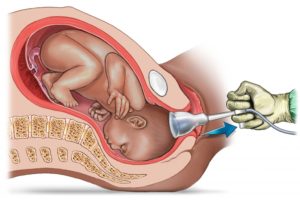
A vacuum extraction is a procedure sometimes done during the course of vaginal childbirth. A vacuum-assisted delivery involves attaching a soft cup to the head of the infant while it is in the birth canal and a hand-held pump is used to create suction to facilitate delivery.
- The advantage is that this assisted birth option has a lower risk than a C-section of prolonged fetal distress.
- The risks of this method include minor scalp injuries or more serious trauma or bleeding of the head.
Forceps Delivery
A forceps delivery is a type of operative vaginal delivery. It’s sometimes needed in the course of vaginal childbirth. A forceps-assisted delivery means that curved instruments are used to facilitate the progress of the infant in the birth canal. Forceps cannot be used if the infant is breech, but it can be an option if the mother is too exhausted or if the infant has to be delivered more quickly than is naturally occurring.
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. The purpose of this website is to promote broad consumer understanding and knowledge of various health topics. It is not intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition or treatment and before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Resources:
https://www.medicinenet.com/7_childbirth_and_delivery_methods/article.htm#what_is_a_water_birth
What You Need to Know When You’re Pregnant with A Rainbow Baby
When you see that second pink line on a pregnancy test, your whole life transforms in the blink of an eye. Having a baby is an experience unlike any other in your lifetime, and you are filled with joy, hope, and expectation. Alongside this joy though, comes the fear of miscarriage, stillbirth, or loss of the baby you’ve dreamed about so fervently.
You may have seen beautiful pictures of babies draped in rainbow wraps or mothers proudly displaying rainbow T-shirts, clothing, and other memorabilia, but never really understood what they were talking about. What exactly is a ” rainbow baby?”
What is a Rainbow Baby?
A rainbow baby is a baby born shortly after the loss of a previous baby. A pregnancy loss could be a miscarriage or a stillbirth (which is typically defined as a baby that has passed away after 20 weeks). The baby that the parents have after the pregnancy that was a loss is called a rainbow baby. Just like the light of a rainbow only appears after the darkness of a rainy sky, a rainbow baby happens after the pain of a loss.
What to Expect If You Are Expecting a Rainbow Baby
Having a baby soon after losing one brings a slew of emotions, and many rainbow moms will tell you that not all are positive emotions. Many mothers who have weathered the loss and gone on to have another baby feel a tremendous sense of self-doubt and guilt at times. They fear that others will think they have gotten over their previous loss, or that they have moved on or replaced their baby. They fear that having a rainbow baby after stillbirth in some way dishonors their baby who has passed and that the joy of the next baby will prevent the mother from properly grieving.
If you are pregnant with a rainbow baby, you will probably experience a lot of different emotions. Many women will have fear and anxiety during their pregnancies after a loss and worry that they will have another miscarriage or that something may be wrong with the baby.
Talking with a doctor who knows your history and asking for certain accommodations, such as working with an ultrasound tech who will be sensitive to your fears, can be helpful. Some women may choose not to disclose their pregnancies to avoid difficult conversations and other women may want to let her family and friends know early on in her pregnancy for emotional support throughout the journey. Every woman is different and what you tell others about your pregnancy is entirely up to you.
The mom’s grief will not necessarily end with the arrival of a rainbow baby.
The significance of a rainbow baby
Pregnancy losses can be devastating, but most women go on to mother again. In doing so, they face the complicated emotional journey of mothering after a miscarriage or stillbirth.
How to Support Your Partner
It’s important to maintain an open line of communication throughout her pregnancy. You may not have physically experienced pregnancy, but the loss was still yours and it’s healthy to discuss how the loss of the pregnancy may have affected you and how you are feeling now.
- Offer unconditional support – Listen without offering advice or suggesting that she feel any one way about her loss or her rainbow pregnancy.
- Honor her as a mother – Remember that she feels like a mother even though her baby is no longer here. Embracing her motherhood may be important and healing for her. Even for mamas who miscarry early in pregnancy, their identity as a mother cannot be erased after a loss.
- Know that grief is an ongoing, lifelong process – Don’t expect mamas to stop grieving a pregnancy loss once a rainbow baby arrives. Resist saying things like “you’ll get pregnant again” or “you’ll have another baby” to comfort her.
Navigating grief and remembering the loss
As time passes, it’s important for many parents to honor and certain dates associated with pregnancy loss. Due dates, birth dates, and death anniversaries are especially poignant. Grief knows no timeline. Many families will choose to acknowledge these dates and the existence of their angel baby long after a loss occurs.
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. The purpose of this website is to promote broad consumer understanding and knowledge of various health topics. It is not intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition or treatment and before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Resources: https://www.verywellfamily.com/what-to-expect-when-pregnant-with-a-rainbow-baby-4112638