High-Risk Pregnancy
A pregnancy is considered high-risk when there are potential complications that could affect the mother, the baby, or both. High-risk pregnancies require management by a specialist to help ensure the best outcome for the mother and baby.
If you’re being treated for a lifelong (chronic) condition, you may have known for a long time that becoming pregnant carries additional risks. Or you may find out you have a high-risk pregnancy because of a problem that develops for the first time during pregnancy. having a high-risk pregnancy means it’s more likely that you or your baby will have health problems during pregnancy, birth, or after delivery. These could be minor problems, but in some cases, a high-risk condition can be life-threatening for a woman or her baby. 
Risk Factors for High-Risk Pregnancy
Reasons that a pregnancy may be considered high risk include:
- Blood disorders. If you have a blood disorder, such as sickle cell disease or thalassemia, the additional strain pregnancy puts on your body can make your condition worse. There are also potential risks to your baby (both during pregnancy and after delivery) if she inherits your condition.
- Chronic kidney disease. This condition increases your risk of miscarriage, developing high blood pressure and preeclampsia, and having your baby early. Pregnancy can also put an extra strain on your kidneys.
- HIV or AIDS. If you have HIV or AIDS, your baby can become infected before birth, during delivery, or when you breastfeed. Fortunately, medication can dramatically reduce this risk.
- Lupus. Lupus and other autoimmune diseases can increase your risk of preterm delivery, preeclampsia, and have a small baby. Being pregnant may also increase the likelihood of your disease flaring up or getting worse.
- Maternal age. Your age can affect how likely you are to have a high-risk pregnancy. Being an older mom (age 35 or older in your first pregnancy) or a younger one (in your teens) puts you at greater risk of some complications and health problems.
- Obesity. Having a body mass index (BMI) of 30 or higher before pregnancy puts you at greater risk of gestational diabetes, type 2 diabetes, and high blood pressure during your pregnancy. When it comes to giving birth, you’re more likely to need your labor induced or a cesarean delivery.

- Thyroid disease. Both an underactive thyroid (hypothyroidism) and an overactive thyroid (hyperthyroidism) during pregnancy can cause problems for you and your baby if the condition isn’t controlled. These problems can include miscarriage, preeclampsia, low birth weight, and having your baby early.
- Type 1 or type 2 diabetes. If your diabetes isn’t managed well, you could be at risk of complications including birth defects, high blood pressure, having your baby early, and having a very big baby. Your baby may have problems with breathing, low glucose levels, and jaundice.
Pregnancy-related issues:
Often a pregnancy is classified as high risk because of issues that arise from the pregnancy itself and that have little to do with the mother’s health. These include:
- Premature Labor is also called preterm labor. It’s when your body starts getting ready for birth too early in your pregnancy. Labor is premature if it starts more than three weeks before your due date. Many factors have been associated with an increased risk of preterm labor, however, including Previous preterm labor or premature birth, particularly in the most recent pregnancy or in more than one previous pregnancy. Pregnancy with twins, triplets or other multiples. Problems with the uterus, cervix or placenta
- Multiple births mean you are carrying more than one baby (twins, triplets, quadruplets, etc.). Multiple pregnancies, which are more common as women are using more infertility treatments, increase the risk of premature labor, gestational diabetes, and pregnancy-induced high blood pressure.
- Placenta Previa is a problem of pregnancy in which the placenta grows in the lowest part of the womb (uterus) and covers all or part of the opening to the cervix. The placenta grows during pregnancy and feeds the developing baby. If the placenta still covers the cervix close to delivery, the doctor may schedule a cesarean section to reduce bleeding risks to the mother and baby.
- Fetal problems, which can sometimes be seen on ultrasound. Approximately 2% to 3% of all babies have a minor or major structural problem in development. Sometimes there may be a family history of fetal problems, but other times these problems are completely unexpected.
How does being high-risk affect my labor?
It’s worth preparing yourself for the idea that the birth you have may not be the birth you’d choose. If your pregnancy is high-risk, you won’t have the option of a home birth or attending a birth center. You’ll need to give birth in a hospital where you and your baby can be monitored closely and specialist care is available during the birth and afterward.
If you’re having multiples, you’re more likely to go into labor early. Preterm labor is also more likely if you have a high-risk pregnancy for other reasons, such as having too much amniotic fluid around the baby or having certain medical conditions. You may also need to have your labor induced to prevent or reduce health problems for you and your baby. Or there may be reasons why a vaginal birth isn’t possible and you need to have a cesarean section.
Talk to your provider about what you can expect during labor, so you can prepare yourself in the best way possible.
Will my baby be okay if I’m high-risk?
 If you have a high-risk pregnancy, one of your biggest worries will probably be whether any harm will come to your baby. It’s natural to be concerned. However, with good prenatal care, it’s possible to have a healthy baby. Healthy moms grow healthy babies: Some conditions, as well as the drugs that are usually prescribed to manage them, pose a risk to your baby’s health. But stopping medications that you take for a condition can also be very dangerous.
If you have a high-risk pregnancy, one of your biggest worries will probably be whether any harm will come to your baby. It’s natural to be concerned. However, with good prenatal care, it’s possible to have a healthy baby. Healthy moms grow healthy babies: Some conditions, as well as the drugs that are usually prescribed to manage them, pose a risk to your baby’s health. But stopping medications that you take for a condition can also be very dangerous.
If your baby is born early, he could have difficulty breathing or feeding, or develop infections or other complications. If this happens, he needs extra care and support, which means staying in the hospital for several weeks, probably in a Neonatal Intensive Care Unit (NICU).
How can I reduce the risk of pregnancy complications?
Find out all you can about your condition and what you can do to stay healthy. Ask your provider for information. At your first prenatal visit, tell your provider about any current health problems you have, any medication you’re taking, and any difficulties you had in previous pregnancies. Have a healthy lifestyle: Follow your provider’s nutritional guidance, gain the right amount of weight, and stay active if you’re able. Don’t smoke or drink alcohol.
Ask your partner, family, and friends for support – this is likely to be a stressful time. Look after your emotional well-being. Take time out for yourself and reduce your stress levels where you can.
If your pregnancy is considered high risk, your doctor may refer you to a perinatologist. Also called a maternal-fetal medicine specialist, a perinatologist is an Obstetrician with special training in high-risk pregnancy care. This specialist will work with your other doctors, nurses, and other health-care professionals to ensure the best possible outcome for both you and your baby.
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. The purpose of this website is to promote broad consumer understanding and knowledge of various health topics. It is not intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition or treatment and before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Resources:
https://www.webmd.com/baby/managing-a-high-risk-pregnancy#1
Does “Pregnancy Brain” Exist?
Pregnancy brain typically refers to lapses in attention and memory. About 80 percent of new mothers report difficulties remembering things that once came naturally, and although not all studies support this, the weight of the evidence shows that during pregnancy, women exhibit measurable declines in important cognitive skills.
Pregnant women are also better at recognizing fear, anger, and disgust. This enhanced ability to identify and discriminate among emotions may help mothers to ensure their infants’ survival. Research from my laboratory has shown that the hormone exposures in pregnancy—for example, high levels of estrogens and oxytocin—are associated with heightened maternal responsiveness and sensitivity to the environment and infants’ needs.
“Relax, pregnancy does not change your brain. But it may affect how mentally sharp you feel.”
Pregnancy Brain a Myth or a Reality?
Fortunately (or unfortunately, depending on how you look at it), there’s no scientific research that proves you get flakey during pregnancy. But even if “pregnancy brain” is just a myth, there are still tons of women who complain of feeling more forgetful or spaced out during their pregnancy.
Pregnancy does not change a woman’s brain even though some women don’t feel as sharp as usual when they’re pregnant.
What Causes “Momnesia?”
If you’re experiencing memory lapses or periods of forgetfulness, chances are your fellow moms-to-be can relate. So what’s to blame? Hormonal changes, lack of sleep, and/or the distractions of spending a lot of time thinking (and stressing) about the baby are the likely causes. Surging hormone levels and new priorities may help explain why pregnancy brain happens.
What Pregnancy Brain Feels Like
Pregnancy brain is “the feeling of walking into a room, going after something, and not remembering what you went for about five to 10 times a day. Many pregnant women and new moms spend a lot of time thinking about the changes that having a baby will bring or taking care of their newborn. As a result, their short-term memory may suffer.
How to Help Your Memory
After the baby arrives, sleep deprivation is clearly a contributing factor. Brizendine says, “Women accumulate up to 700 hours of sleep debt in the first year after having a baby and that causes the brain not to be at its best for things other than caring for the baby.”
Save your sanity by writing things down and making lists, along with snacking regularly and getting lots of rest. Also, be sure to take your prenatal vitamins —they contain ingredients that help boost mental sharpness. Don’t worry, it’s annoying, but it isn’t permanent.
Pregnancy primes the brain for dramatic neuroplasticity, which is further stimulated by delivery, lactation and mother-child interactions. Some evolutionary biologists have argued that the development of maternal behaviors is the primary force shaping the evolution of the mammalian brain. Of interest, these alterations may become more pronounced with each successive pregnancy and persist throughout a mother’s lifespan. But helpful adaptations are rarely achieved without an associated cost—and pregnancy brain may reflect just such a cost.
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. The purpose of this website is to promote broad consumer understanding and knowledge of various health topics. It is not intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition or treatment and before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Resources:
https://www.webmd.com/baby/features/memory_lapse_it_may_be_pregnancy_brain#1
Importance of Genetic Testing Before & During Pregnancy
All soon-to-be parents want their children to be healthy and to have a pregnancy free of major complications. Unfortunately, complications can occur during pregnancy, either with the mother’s health or the child’s. Sometimes, the mother and child are at risk for certain complications throughout the pregnancy because of their family history and genetics.
 All pregnant women are offered some form of testing for genetic problems. Now, deciding whether you want to have it done is completely personal. You will want to weigh different factors, including baby’s risk for genetic problems.
All pregnant women are offered some form of testing for genetic problems. Now, deciding whether you want to have it done is completely personal. You will want to weigh different factors, including baby’s risk for genetic problems.
What is genetic testing (carrier screening)?
Carrier testing is a type of genetic testing that is used to determine if a person is a carrier for a specific autosomal recessive disease. This kind of testing is used most often by couples who are considering becoming pregnant to determine the risks of their child inheriting one of these genetic disorders. In other words, if you screen positive for a genetic abnormality but your partner does not, your child will not inherit the condition. And even if you both screen positive, there’s only a 25 percent chance your baby will have the disease.
When should you get genetic testing?
Getting screened before you try to get pregnant can give you reassurance (if you or your partner is not a carrier, it’s one less thing to worry about when do you get pregnant) or can help you make an informed game plan for pregnancy. If it turns out that you are both carriers, you can be prepared for and bone up on what it means to have a baby with the genetic condition, choose to learn about certain prenatal tests to check whether your baby’s healthy, or you can consider other options like egg or sperm donation or adoption.
Getting tested once you become pregnant (if you hadn’t done so ahead of time) can help you and your doctor decides the right prenatal tests for your baby, and what to look for if you choose to have them. If you know that your baby’s at an increased risk for having cystic fibrosis or sickle cell disease, for instance, your doctor can look for those conditions specifically through either a CVS (chorionic villi sampling) or amniocentesis.
Who are genetic carriers?
If both partners in a couple carry the same recessive disease, then the couple have a one in four chance of a child with that disease. Carrier couples may, therefore, have multiple affected children. Some recessive diseases are relatively mild but others are severe, including many that cause death at or shortly after birth.
What are some of the most common genetic diseases? 
- Cystic fibrosis is a life-threatening condition that causes lung damage and digestive problems. It is a progressive, genetic disease that causes persistent lung infections and limits the ability to breathe over time. In people with CF, a defective gene causes a thick, sticky buildup of mucus in the lungs, pancreas, and other organs.
- Sickle cell disease is a disorder of the blood caused by an inherited abnormal hemoglobin (the oxygen-carrying protein within the red blood cells). The abnormal hemoglobin causes distorted (sickled) red blood cells. The sickled red blood cells are fragile and prone to rupture, most common in people of African and Mediterranean backgrounds, cause a blood disorder that leads to anemia, a weakened immune system, and other health complications.
- Thalassemia is another blood disorder common to people of African and Mediterranean descent. It is an inherited blood disorder in which the body makes an abnormal form of hemoglobin. Hemoglobin is the protein molecule in red blood cells that carries oxygen. The disorder results in excessive destruction of red blood cells, which leads to anemia and bone growth and liver problems; in severe cases, some babies born with the condition may not survive.
- Tay-Sachs Disease, which mainly affects people of French Canadian and Eastern European Jewish descent, is a disorder of the central nervous system that’s usually fatal in early childhood. Eastern European Jews also face an increased risk for another nervous system disorder called Canavan disease as well as a number of other conditions including familial dysautonomia, familial hyperinsulinism, and Gaucher disease. Your doctor can screen for all of these conditions at the same time.
- Fragile X Syndrome is a genetic condition that causes a range of developmental problems including learning disabilities and cognitive impairment and mental retardation. Usually, males are more severely affected by this disorder than females. Affected individuals usually have delayed development of speech and language by age 2. It is not linked to a specific ethnic background. Reviewing your family’s health history with a doctor or genetic counselor may help you decide whether you should be screened for Fragile X.
Benefits
 When pre-pregnancy carrier screening programs are introduced, they reduce death and disease associated with screened diseases. They can save families from experiencing the tragedy of a child affected by a significant genetic disease. They also reduce the burden of recessive disease with the population as a whole. Each recessive disease is rare but there are hundreds of recessive diseases and so collectively they have wide-ranging social and economic impacts.
When pre-pregnancy carrier screening programs are introduced, they reduce death and disease associated with screened diseases. They can save families from experiencing the tragedy of a child affected by a significant genetic disease. They also reduce the burden of recessive disease with the population as a whole. Each recessive disease is rare but there are hundreds of recessive diseases and so collectively they have wide-ranging social and economic impacts.
So pre-pregnancy carrier screening programs that include many genetic diseases, as now recommended by the American College, would maximize knowledge of genetic risk for couples.
Limitations
When testing genes, some identified variations are definitely harmful while most are definitely harmless. But for some variations, we can’t be sure if they are harmful, and whether or not they will cause disease in any children. There is no guarantee that pre-pregnancy screening will result in a healthy baby, but it will allow couples options to reduce the burden of disease associated with known disease-causing mutations.
Counseling is required before and after the test to explain the risks to couples.
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. The purpose of this website is to promote broad consumer understanding and knowledge of various health topics. It is not intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition or treatment and before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Resources:
What Causes Pregnancy Cravings
Pregnancy and food cravings go hand in hand: Food cravings are sudden urges to eat a particular type of food. They are a real phenomenon and affect many women during pregnancy.Many of these cravings seem to come out of nowhere, and they can feel overpowering. What causes them? Hormones, right?
There’s no scientific explanation for food cravings. There’s no data saying that what a woman craves is related to something her body or her baby needs, and there’s no data to support that typical pregnancy food cravings are harmful, either.
There are three facts about the wonderful world of pregnancy that we all know to be true
- A woman can have one or more tiny humans floating around in her belly.
- After nine-ish months said tiny human will emerge from the woman’s body — naked, bloody, and possibly crying.
- During the nine-ish months, the woman is allowed to eat EVERYTHING she wants. No matter how weird it might be.
Why do cravings develop?
No one really knows why food cravings develop. It seems logical that cravings might be due to something lacking in the diet, or an increased need for certain vitamins and minerals. However, there is no evidence of a link between cravings and nutrient deficiency.
Ways to Stop Cravings
- Get enough sleep. Loss of sleep increases hunger during the day, which leads to cravings. Getting the right amount of shut-eye could stop cravings.
- Eat a healthy breakfast. For some people, cravings are part of a cycle of blood sugar highs and lows that can be kicked off almost the moment their feet hit the floor in the morning. A breakfast featuring fiber and protein is more likely to control this cycle. Consider a scrambled egg on whole-wheat bread or a turkey sandwich instead of sugary cereal or a Danish.
- Eat meals at scheduled times. The secret to stopping cravings is to manage hunger and “only eating at set times — no casual eating.
- Make the foods you crave difficult or impossible to get to. No matter how much you love brownies, if you don’t keep any at home or at work, chances are your craving will pass unsatisfied. Instead, make healthy alternatives easy to access in your eating plan and prepare ahead for those times when you’ll need a healthy snack within easy reaches, like when you’re on the road.
- Keep a food journal. This may not totally stop cravings, but it could keep you from acting on them if the thought of writing down the calorie and fat content of a steak is more painful than going without it. A food journal will also help you identify the times of day when your cravings are the strongest.
- Identify your craving triggers. Emotional eating is a real phenomenon. If you pay attention, you may find that your cravings are worse when you are stressed or depressed. Managing those situations will help stop cravings.
- Eat a varied diet. Sticking to the tried-and-true may help you count calories, but it could also leave you feeling unfulfilled. People need variety in their diets, so try new dishes or combinations of foods to stop cravings. Just because you’re on a diet doesn’t mean it can’t be satisfying.
Foods to avoid 
When you are pregnant, there are a number of foods that should avoid. Things like soft cheeses, sushi, raw eggs and undercooked meat can contain harmful bacteria, including salmonella and E. coli. and lead to harmful illnesses such as listeria or toxoplasmosis.
Pregnancy facts aren’t so scientific, but it summarizes what many of us know about pregnancy, especially when it comes to eating. Food cravings are a common occurrence during pregnancy.
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. The purpose of this website is to promote broad consumer understanding and knowledge of various health topics. It is not intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition or treatment and before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Resources:
https://www.pregnancybirthbaby.org.au/food-cravings-during-pregnancy
What Happens To A Woman’s Body During Childbirth
The human body is an amazing thing. It’s ability to fend off disease, perform essential functions, and harbor life until birth are a few of the most important, and amazing, feats that the human body is capable of. From the moment of conception, a woman’s body immediately begins to change in order to accommodate the internal growth of a child. As the pregnancy progresses, a woman’s body adapts to the needs of both the mother and child.
Childbirth is challenging and complications occur, but women’s bodies are designed to give birth. The shape of the pelvis, hormones, powerful muscles and more all work together to help you bring your baby into the world – before, during and after childbirth.
As you approach the time of birth, your contractions draw the cervix up into the body of the uterus, and it becomes thinner (called effacement) and opens (called dilation). When the cervix is fully dilated (about ten centimeters), contractions help the baby begin to move from the uterus into the vagina.
The First Trimester
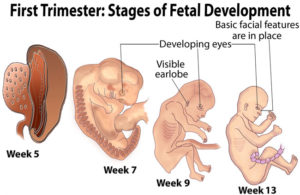 The first trimester is the time in between fertilization of the egg by the sperm (conception) and week 12 of a pregnancy. A woman’s body goes through many changes during the first 12 weeks of a pregnancy. a mother’s body is building storing nutrients and trying to keep up with the demands of a growing fetus. Fatigue is a normal reaction and is often the most inhibiting during the first trimester. Physical attributes may include constipation, heartburn, breast changes, and vaginal changes.
The first trimester is the time in between fertilization of the egg by the sperm (conception) and week 12 of a pregnancy. A woman’s body goes through many changes during the first 12 weeks of a pregnancy. a mother’s body is building storing nutrients and trying to keep up with the demands of a growing fetus. Fatigue is a normal reaction and is often the most inhibiting during the first trimester. Physical attributes may include constipation, heartburn, breast changes, and vaginal changes.
The Second Trimester 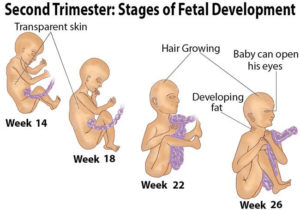
The second Trimester is the best part of pregnancy. The span from week 13 to week 27 of pregnancy is called the “honeymoon period” for good reason: Typically, nausea subsides, emotions even out and sex drive returns. It’s also the time when you’ll start to feel the baby’s first movements.
The Third Trimester
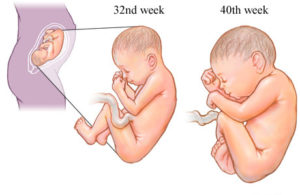 The third trimester of your pregnancy is from week 29 to week 40 – months seven, eight and nine.Your baby continues to grow, and as the third trimester progresses she’ll have a better chance if she’s born early. The end of your pregnancy is in sight. It won’t be long until your baby arrives. Feelings at this stage of pregnancy tend to vary from tiredness and worry to excitement about the baby.
The third trimester of your pregnancy is from week 29 to week 40 – months seven, eight and nine.Your baby continues to grow, and as the third trimester progresses she’ll have a better chance if she’s born early. The end of your pregnancy is in sight. It won’t be long until your baby arrives. Feelings at this stage of pregnancy tend to vary from tiredness and worry to excitement about the baby.
How does your body prepare for labor?
Braxton Hicks contractions
Braxton Hicks contractions are intermittent uterine contractions that start in early pregnancy, although you probably won’t notice them until sometime after mid-pregnancy. (Some women never notice them.) As your pregnancy progresses, Braxton Hicks contractions tend to occur somewhat more often, but until you get to your last few weeks, they’ll probably remain infrequent, irregular, and painless.
Changes to the cervix
As labor gets closer, your cervix softens and becomes thinner, getting ready for the dilation (widening) that will allow the baby to enter the vagina. You may also see a ‘show’ which is a pinkish plug of mucus, stained with blood.
Engagement
Your baby may move further down your pelvis as the head engages, or sits in place over your cervix, ready for the birth. Some women feel they have more room to breathe after the baby has moved down. This is called ‘lightening’.
Rupture of the membranes, or ‘waters breaking’
Rupture of the membranes is known colloquially as “breaking the water” or as one’s “water breaking”. A premature rupture of membranes (PROM) is a rupture of the amnion that occurs prior to the onset of labor. Sometimes, a child is born with no rupture of the amniotic sac (no rupture of membranes).
Some women find the sac of amniotic fluid containing the baby breaks before labor, contractions start and the fluid runs (or gushes) out of the vagina. If your waters have broken but you have not started having regular contractions within 24 hours, you may need your labor to be induced because there is a risk of infection. Your midwife or doctor will talk to you about this.
How the pelvis is designed for childbirth 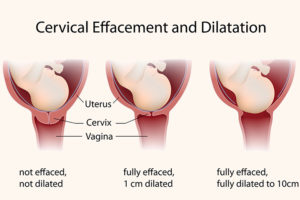
The female pelvis is the bony cradle that holds and even rocks your baby while she is developing in the uterus. It is amazingly designed for its functions, especially for giving birth.
The pelvis is well-designed to carry the weight of both the mother and baby. It connects the vertebrae and the lower limbs and protects the reproductive organs, the bladder, intestines, and rectum. It also provides attachment for the abdominal muscles and the muscles of the pelvic floor.
The pelvis is made up of four bones: the two large hip bones that form the sides of the cradle and meet at the front and the sacrum and coccyx at the back.
During pregnancy hormones cause the ligaments soften and stretch causing a slight separation of the joints, which allows flexibility for the baby’s head to pass through during birth. Sometimes pregnant women may experience some pelvic pain and discomfort as a result of this loosening of the joints.
The Childbirth Process
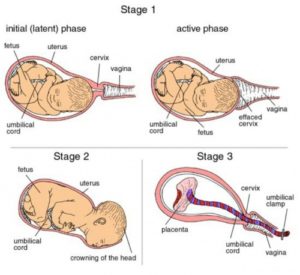 Childbirth, also known as labor and delivery, is the ending of a pregnancy by one or more babies leaving a woman’s uterus by vaginal passage or C-section. It involves three stages of labor: the shortening and opening of the cervix, descent, and birth of the baby, and the delivery of the placenta.
Childbirth, also known as labor and delivery, is the ending of a pregnancy by one or more babies leaving a woman’s uterus by vaginal passage or C-section. It involves three stages of labor: the shortening and opening of the cervix, descent, and birth of the baby, and the delivery of the placenta.
Cervical dilation occurs during active labor, making room for the baby to travel through the birth canal. The cervix dilates naturally when the body is ready to give birth, but when it’s necessary to move things along more quickly, dilation may be stimulated using medications or mechanical techniques.
The placenta is delivered as part of the afterbirth with a small gush of blood, from a few minutes to a half hour after the baby arrives. The doctor or midwife will examine it to make sure it’s intact and that nothing has been left behind in the uterus.
When childbirth doesn’t go to plan
Unfortunately, not everything goes to plan during birth. Sometimes your maternity team may need to intervene to assist in the delivery of your baby. Find out more about how your doctor or midwife may assist during your labor and what happens when your baby is premature or unwell.
Sometimes labor can be induced (started artificially) if your baby is overdue or there is any sort of risk to you or your baby’s health, for example, if you have high blood pressure or if your baby is failing to grow and develop.
In rare cases, a mother may experience cephalopelvic disproportion (CPD), which is when the baby’s head is too big to fit through the pelvis. A diagnosis of CPD is usually made when labor hasn’t progressed and synthetic oxytocin has not helped. A cesarean is usually the next step.
In conclusion, The stages of pregnancy and childbirth may seem daunting at times. However, they are some of the most rewarding phases of life. Bringing a child into this world is a beautiful labor.
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. The purpose of this website is to promote broad consumer understanding and knowledge of various health topics. It is not intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition or treatment and before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Resources:
https://www.pregnancybirthbaby.org.au/what-happens-to-your-body-in-childbirth
http://positivemed.com/2015/10/27/what-happens-to-a-womans-body-during-childbirth/
Different Positions of a Baby in the Womb
Unborn babies toss and turn and hold many different positions within the womb during the gestation period; pregnant women everywhere will attest to the fact that their children always start up the gymnastics at bedtime. When the due date nears, the importance of the baby’s position becomes less of a joke and a serious point of discussion. The different positions that your baby may take in the womb will play a role in how he is born.
Head-Down
Most babies flip and turn with great frequency throughout pregnancy but generally end up in the “head-down” position around the 33 to 36-week range, according to the American Pregnancy Association. Head-down literally means that the baby’s head is pointing toward the birth canal, and his feet, when his legs are fully extended, are in the vicinity of his mother’s ribs. Babies at this advanced gestational age most commonly stay in the head-down position for the remainder of the pregnancy and may not move as much as in the earlier months, mainly due to space constraints.
Breech 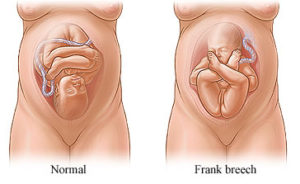
Breech is the position in which the baby’s buttocks or feet are nearest to the birth canal. A breech baby’s head is close to her mother’s ribs. This position is less desirable than the head-down position for birth, and breech babies have an increased risk of birth defects or trauma during the birth. Your doctor may try to turn the baby around in a procedure called a version, deliver the baby in a breech position or perform a cesarean section. Abnormalities in the baby’s anatomy or the shape of your uterus may prevent the baby from turning around.
There are three variations of a breech presentation:
- Complete breech: When the buttocks are pointing toward the birth canal (downward), with the legs folded at the knees. The feet are near the buttocks.
- Frank breech: The buttocks are toward the birth canal, but the baby’s legs are straight up in front of their body and the feet are near the head.
- Footling breech: One or both of the baby’s feet are pointing downward toward the birth canal.
Transverse
 A baby that lies sideways in his mother’s womb is in a horizontal position. The baby’s head may point to the left side of your body and the feet to the right, or vice versa. Transverse positioning at the time of birth is extremely rare; only one out of 2,000 babies takes a transverse position. Like breech presentation, a baby who lies sideways may not be able to turn around due to structural abnormalities in the uterus. Pregnancy Today explains that babies who are transverse are delivered by cesarean section to ensure a safer delivery.
A baby that lies sideways in his mother’s womb is in a horizontal position. The baby’s head may point to the left side of your body and the feet to the right, or vice versa. Transverse positioning at the time of birth is extremely rare; only one out of 2,000 babies takes a transverse position. Like breech presentation, a baby who lies sideways may not be able to turn around due to structural abnormalities in the uterus. Pregnancy Today explains that babies who are transverse are delivered by cesarean section to ensure a safer delivery.
Risk Factors for Transverse Lie
Women with the following conditions are at a high risk for transverse presentation:
- A high ratio of amniotic fluid to a fetus
- Uterine abnormality
- Placenta previa
- Fibroids in the uterus
- Factors preventing fetal head engagement in the mother’s pelvis
- Narrow or contracted pelvis
- More than 2 babies in the womb
Diagnosis of Transverse Presentation
Abdominal examination— In transverse position, the presenting part of the fetus is typically the shoulder. During an abdominal examination, the head or the buttocks cannot be felt at the bottom of the uterus and the head is usually felt on the side.
Vaginal examination— A shoulder may be felt during a vaginal examination. An arm of the fetus may even slip forward and the hand or elbow may be felt during the pelvic examination.
Confirmation – An ultrasound scan of the uterus confirms the transverse lie position.
Complications of Transverse Lie
A transverse presentation can cause serious complications during delivery. Some of the consequences are listed below:
- Obstructed labor
- Umbilical cord or hand prolapse
- Postpartum hemorrhage
- Birth trauma
- Rupture of the uterus
Posterior
Babies in the head-down position most often enter the world with their faces facing their mothers’ backs. Posterior is the term used to describe a baby in the head-down position with her face facing the mother’s stomach, in other words with her face turned up. The altered positioning of the baby’s body may lead to back labor in the mother, rather than cramping in the abdomen.
Can I turn my baby?
Occasionally, a baby may not end up in the correct position for delivery. It’s important to know if your baby isn’t in the occipito-anterior position right before birth. Depending on the exact position, it could lead to complications during delivery. There are some methods you can use to coax your baby into the right position.
You can try the following ideas:
- When you sit down, tilt your pelvis forward instead of backward.
- Spend time sitting on a birth ball/exercise ball.
- Make sure your hips are always higher than your knees when you sit.
- If your job requires lots of sitting, take regular breaks to move around.
- In your car, sit on a cushion in order to lift up and tilt your bottom forward.
- Get on your hands and knees (like you are scrubbing the floor) for a few minutes at a time. Try this a few times a day to help move your baby into the anterior position.
Unfortunately, these tips don’t always work. If your baby stays in a posterior position when labor starts, it may be because of the shape of your pelvis rather than your posture. In some cases, a cesarean delivery will be necessary.
Resources:
https://www.healthline.com/health/pregnancy/baby-positions-in-womb#turning-baby
https://www.livestrong.com/article/204490-different-positions-of-a-baby-in-the-womb/