10 Signs of Approaching Labor
While there are characteristic changes in the body with impending labor, every woman’s experience is unique and different. “Normal” can vary from woman to woman. The signs and symptoms of normal labor can begin three weeks prior to the anticipated due date up until two weeks afterward, and there is no precise way to predict exactly when a woman will go into labor.
“It’s the event you’ve been happily (and nervously) anticipating for months: Your baby’s birth! “
How will you know when it’s time to grab your hospital bag and get to the delivery room? Thankfully, your body will give you some solid clues.
Here are 10 common signs that labor is near.
- The baby drops
Medically known as “lightening,” this is when the baby “drops.” The baby’s head descends deeper into the pelvis and is getting into position to make his exit. For some women, this occurs up to 2 weeks prior to the beginning of labor; other women may not notice this event at all. In subsequent births, this “lightening” doesn’t often happen until you’re truly in labor.
- An increased urge to urinate
An increased urge to urinate can be a result of the baby’s head dropping into the pelvis. The low position of the baby’s head puts even more pressure on the urinary bladder, so many women approaching labor might feel a frequent need to urinate. As the baby drops, breathing can become easier since there is less pressure on the diaphragm from underneath.
- The mucus plug passes
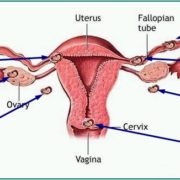
Passage of the mucus plug is a known sign that labor is near. Thick mucus produced by the cervical glands normally keeps the cervical opening closed during pregnancy. This mucus plug must be expelled before delivery. It can come out in one large piece (it looks similar to the mucus in your nose) or lots of little ones, though you may not get a glimpse of it at all and some women don’t lose it before delivery. Pressure from the baby’s head causes the mucus plug to be expressed from the vagina, sometimes as blood-tinged vaginal discharge (referred to as “bloody show”) and is a good indication that labor is imminent, but without contractions or dilation of three to four centimeters, labor could still be a few days away.
- The cervix dilates
Your cervix, too, is starting to prepare for birth. Dilation of the cervix is a sign that labor is approaching, although this is detected by the health-care professional during a pelvic examination. This begins in the days and even weeks prior to the onset of labor; “Fully dilated” means the cervix has dilated to a width of 10 cm. But everyone progresses differently, so don’t be discouraged if you’re dilating slowly or not at all yet.
- Thinning of the cervix
In addition to dilation, thinning (effacement) of the cervix also occurs. This occurs in the weeks prior to labor, since a thinned cervix dilates more easily. This sign is also detected by the health-care professional during a pelvic exam.
- Back pain
Contractions can often begin in the back and move forward to the pelvis. And some women do experience “back labor,” which is characterized by severe discomfort in the lower back that is most intense during contractions and often painful between contractions. Women also notice loosening of the joints, particularly in the pelvic area, as the third trimester progresses, in preparation for delivery.
- Contractions
It’s inevitable—at some point, you’ll realize that crampy feeling you’re having might be more than just cramps. They’ll change to regular contractions, which indicate your body is beginning the process of a birthing baby. Contractions, which can vary among women and can be described as pounding, tightening, stabbing, or similar to menstrual cramps, increase in strength and frequency as labor approaches.
Irregular contractions, known as Braxton-Hicks contractions or “false labor” occurs toward the end of pregnancy during the third trimester. Braxton-Hicks contractions are usually milder than those of true labor, and they do not occur at regular intervals. The best thing to do? Relax, get comfortable or perhaps take a shower. Time the contractions and head to the hospital or birthing center when they become about five minutes apart.
- Burst of energy
Many women describe feeling a sudden burst of energy and excitement in the weeks prior to labor, in contrast to feeling extra tired as is typical of pregnancy. Often referred to as “nesting,” this impulse often is accompanied by a sense of urgency to get things done or make plans for the baby.
- Nausea and diarrhea
Just as the muscles in your uterus are relaxing in preparation for birth, so too are other muscles in your body, including those in the rectum. And that can lead to diarrhea, that pesky little labor symptom you may well have experienced at other times during pregnancy. Though annoying, it’s completely normal; stay hydrated and remember it’s a good sign!
- Your water breaks
Despite what movies will have us believe, how your water breaks (in other words, how the membranes of the amniotic sac burst) can vary a lot.
If your water breaks and you’re experiencing contractions, this is one of the biggest signs of labor. But if contractions haven’t set in yet, your doctor may want you to wait a few hours before coming in. Rupture of the amniotic membranes, or one’s “water breaking,” usually is a sign that labor has begun. Amniotic fluid should be colorless and odorless. It can sometimes be hard to distinguish from urine, but amniotic fluid does not have an odor. If you are leaking amniotic fluid, it is essential to contact your health-care professional right away.
Should I Call the Doctor?
It’s not necessarily your due date—that’s just an estimate, and there’s really no telling exactly when the baby will arrive. Keep in mind too that some women may deliver before 37 weeks (which would be considered a preterm birth); others, who go past 41 weeks, may wind up getting induced, depending on your doctor and your hospital’s policies.
If you think you’re going into labor, your practitioner should have advised you on what to do when your contractions become regular: “Call me when they’re coming about five minutes apart for at least an hour,” for example. Contractions won’t all be exactly spaced, but if they are becoming pretty consistent, more painful and longer (usually around 30 to 70 seconds), it’s time to check in with your doc. If you think you might be in labor but aren’t sure, get on the phone; your provider can advise you on what’s going on. Don’t feel embarrassed or worry about calling outside of office hours (your doctor or midwife knew this would happen when she got into the baby-catching business!).
You should always call if:
- You experience any bleeding or bright-red discharge (not brown or pinkish).
- Your water breaks — especially if the fluid looks green or brown; this could be a sign that meconium is present (which is your newborn’s first stool; it can be dangerous if your baby ingests it during birth).
- You experience blurred or double vision, a severe headache, or sudden swelling. These can be symptoms of preeclampsia, which is characterized by pregnancy-induced high blood pressure and requires medical attention.
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. The purpose of this website is to promote broad consumer understanding and knowledge of various health topics. It is not intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or another qualified healthcare provider with any questions you may have regarding a medical condition or treatment and before undertaking a new health care regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Resources:https://www.medicinenet.com/early_signs_and_symptoms_of_labor/article.htm#7_contractions